STANDARD 7

OVERVIEW
Key Messages for Adjunct Treatments
- Adjunct Treatments are used to improve the individual’s ability to fully participate in the Core Treatments
- The costs of Adjunct Treatments should be discussed before adding a treatment to a care plan
- Supports can improve stability and mobilization, conserve energy, minimize the risk of falling and provide options for safe movement to reduce the lower limb loading that can increase pain
- The individual’s pain experience can be influenced by changes in physical, emotional, behavioural, and cognitive states so cognitive behaviour therapy can be offered that may or may not include Acceptance Commitment Therapy (ACT) and mindfulness
- Inter-disciplinary self-management programs offer more specific resources and strategies to help struggling individuals develop coping skills in response to their evolving symptoms
- The algorithm guides progressive use of pharmacological treatments
- The individual’s full history should be considered before prescribing
- Complications, side effects and possible interactions of medications should be considered
- Intra-articular injections includes: steroids, hyaluronic acid and platelet rich plasma
- Advanced pain management includes opioids (use with extreme caution), peripheral nerve blocks or referral for joint surgery
KEY RESOURCES
- Canadian Opioid Prescribing Guidelines
- Arthritis Society Website on Medical Cannabis Use
- Bone and Joint Health SCN White Paper on Stem Cells
- Shared Decision-Making Toolkit
- FORM to Document/Modify a Care Plan for Management of OA
- Tables of Examples for the Treatment Toolbox
- PEER OA Decision Aid
- Health Change Methodology
- Alberta Referral Directory
INTRODUCTION
Core Treatments (Standard 4, Standard 5, and Standard 6) are essential foundations of every care plan and have the strongest evidence for conservative management of osteoarthritis (OA)1-4. However, Adjunct Treatments can be considered if individuals with OA:
1Bowden JL, Hunter DJ, Deveza LA, Duong V, Dziedzic KS, Allen KD, et al. Core and adjunctive interventions for osteoarthritis: Efficacy and models for implementation. Nature Reviews Rheumatology. 2020;16(8):434-47.
2Gay C, Chabaud A, Guilley E, Coudeyre E. Educating patients about the benefits of physical activity and exercise for their hip and knee osteoarthritis. Systematic literature review. Annals of Physical and Rehabilitation Medicine. 2016;59(3):174-83.
3Rice D, McNair P, Huysmans E, Letzen J, Finan P. Best evidence rehabilitation for chronic pain part 5: Osteoarthritis. Journal of Clinical Medicine. 2019;8(11):1769.
4Wellsandt E, Golightly Y. Exercise in the management of knee and hip osteoarthritis. Current Opinion in Rheumatology. 2018;30(2):151-9.
- Find it difficult to participate in Core Treatments
- Report minimal progression toward their goals or
- Require additional support to manage symptoms
Adjunct Treatments are used to improve the individual’s ability to fully participate in Core Treatments. The clinician can provide evidence informed non-pharmacological and pharmacological treatments options to support the individual’s goals. In particular, muscle weakness, joint pain and fear of exacerbating symptoms can be barriers to adhering with prescribed exercise and physical activity (Standard 5). Addressing these physical and emotional barriers with Adjunct Treatments can support:
- Affected joints to ease mobility55Yu SP, Hunter DJ. Managing osteoarthritis. Australian Prescriber. 2015;38(4):115-9.
- Behavioural change11Bowden JL, Hunter DJ, Deveza LA, Duong V, Dziedzic KS, Allen KD, et al. Core and adjunctive interventions for osteoarthritis: Efficacy and models for implementation. Nature Reviews Rheumatology. 2020;16(8):434-47.
- Long-term commitment to exercise and physical activity11Bowden JL, Hunter DJ, Deveza LA, Duong V, Dziedzic KS, Allen KD, et al. Core and adjunctive interventions for osteoarthritis: Efficacy and models for implementation. Nature Reviews Rheumatology. 2020;16(8):434-47.
The clinician may refer to other disciplines with additional skills in OA management and expertise in specific Adjunct Treatments to build and strengthen the individual’s support network. This multidisciplinary care team approach combined with collaboration with the individual will ensure the individual’s priorities, values and preferences are considered when pursuing Adjunct Treatments. Any additional costs of Adjunct Treatments should be considered and discussed with the individual before adding to an OA care plan.
WALKING & ENVIRONMENTAL SUPPORTS
Non-pharmacological Adjunct Treatments include any non-medicinal intervention proven to support symptom management. They are:
- Supports (walking and environmental)1,51Bowden JL, Hunter DJ, Deveza LA, Duong V, Dziedzic KS, Allen KD, et al. Core and adjunctive interventions for osteoarthritis: Efficacy and models for implementation. Nature Reviews Rheumatology. 2020;16(8):434-47.
5Yu SP, Hunter DJ. Managing osteoarthritis. Australian Prescriber. 2015;38(4):115-9. - Cognitive behavioural therapy11Bowden JL, Hunter DJ, Deveza LA, Duong V, Dziedzic KS, Allen KD, et al. Core and adjunctive interventions for osteoarthritis: Efficacy and models for implementation. Nature Reviews Rheumatology. 2020;16(8):434-47./span>
- Inter-disciplinary self-management programs11Bowden JL, Hunter DJ, Deveza LA, Duong V, Dziedzic KS, Allen KD, et al. Core and adjunctive interventions for osteoarthritis: Efficacy and models for implementation. Nature Reviews Rheumatology. 2020;16(8):434-47.
The use of walking supports can improve stability, mobilization, minimize the risk of falling and the severity of injury if a fall does occur, and reduce the lower limb loading that can increase pain. Walking supports include:
| Type | Facts and Benefits | Examples |
|---|---|---|
| Assistive Devices |
|
|
| Braces |
|
|
| Footwear and Orthotics |
|
Note: consider cost vs. benefit. See learn mores for more information. |
The use of environmental supports can conserve energy and provide options for safe movement. Environmental supports include:
| Type | Facts and Benefits | Examples |
|---|---|---|
| Assistive Technologies |
|
|
| Home Adaptations |
|
|
Supports are relatively affordable options that can address symptoms and allow individuals to better participate in exercise and physical activities. If these treatment options are applicable, the Primary Clinician can refer the individual to appropriate supporting clinicians or medical supply stores that are familiar with the walking supports commonly used by people with hip or knee OA. The individual can also self-refer to many clinicians who have supports expertise.
COGNITIVE BEHAVIOURAL THERAPY11Bowden JL, Hunter DJ, Deveza LA, Duong V, Dziedzic KS, Allen KD, et al. Core and adjunctive interventions for osteoarthritis: Efficacy and models for implementation. Nature Reviews Rheumatology. 2020;16(8):434-47.
The individual’s OA pain experience can be influenced by changes in physical, emotional, behavioural, and cognitive states .
Cognitive behaviour therapy can be offered to individuals to:
- Support mental health
- Develop pain coping strategies
- Develop stress and anxiety management strategies
- Promote behavioural modifications
The clinician may offer advice for these or refer the individual to skilled supporting clinicians or other trained cognitive specialists.
SELF MANAGEMENT
Inter-disciplinary self-management programs offer resources and strategies to help individuals develop, adhere to, and modify their goals and course of action in response to their evolving symptoms11Bowden JL, Hunter DJ, Deveza LA, Duong V, Dziedzic KS, Allen KD, et al. Core and adjunctive interventions for osteoarthritis: Efficacy and models for implementation. Nature Reviews Rheumatology. 2020;16(8):434-47.. These programs are more specific and focused than the self-management principles embodied in Core Treatments; the programs are appropriate for an individual who has struggles with employing coping strategies and wants more practice and examples. These programs aim to increase an individual’s confidence to self-manage their symptoms and health outcomes. These programs emphasize the following topic areas:
Empowering individuals to play an active role in identifying what needs to change and set realistic goals including appropriate pace setting.
Helping individuals monitor their progression and changes in symptoms, in order to recognize when they need to ask for additional support.
Evaluation of progress in meeting goals and how to overcome barriers and challenges.
Guidance for managing emotional impacts of OA for individuals and their family support systems.
- Thermotherapy: Heat modalities and cryotherapy to manage joint inflammation; and
- Activity self-selection: Building their understanding of their local structured exercise programs and physical activity options so they can choose new ones as they wish.
When these programs are offered in a group setting, they can also provide an opportunity for individuals to build a support network, and feel less alone (universality). Peer support can improve self-management of OA6,76Ali SA, Walsh KE, Kloseck M. Patient perspectives on improving osteoarthritis management in urban and rural communities. Journal of pain research. 2018;11:417-25.
7Bryk C, Lewis TR, Miller J, Penman C, Teare S. The Experience of Waiting for Help with Osteoarthritis. Calgary, AB: PACER; 2013. Contract No.: Report. .
All education resources and sessions (Standard 4) will be combined with guidance on self-management strategies. The clinician should work with the individual to review and modify self-management strategies on an ongoing basis and as symptoms evolve.
PHARMACOLOGICAL INTERVENTIONS
Pharmacological treatments include three types of medications:
- Non-prescription treatments: topical and oral
- Prescription treatments: topical and oral
- Intra-articular injectables
Pharmacological pain management strategies can be recommended by a primary care physician and/or in collaboration with a pharmacist or nurse practitioner. Prior to making pharmacological treatment recommendations, it is important that the clinician team assess the individual’s:
- Symptoms
- Pain experience
- Comorbidities
- History of pharmacological treatment use
Complications, side effects and possible interactions of the OA with other medicines should also be considered. Further consultation with other medical specialties may be required to ensure safety of the individual with OA prior to making recommendations. Intra-articular injections should be performed by a skilled clinician.
Symptom self-management strategies should be discussed in conjunction with pharmacological treatment planning. Pharmacological treatments should be used to reduce pain symptoms to promote and enable full participation in Core Treatments. Since medications cannot reduce pain to zero and come with the potential for side effects or tolerance development, encourage the individual to combine pharmacological treatments with other non-pharmacological treatments such as thermotherapy or activity self-selection to help optimize pain management.
As symptoms evolve, the pain management strategy must be modified to suit the individual’s current needs. Below is a stepped algorithm for pharmacological treatments that may be used by the clinician when considering options for best relief of the individual’s current pain symptoms. The individual’s needs, preferences, values, blood pressure, risks of side-effects and socio-economic status must be discussed when making pharmacological treatment choices. Selection of pharmacological treatments will influence the follow-up plan the clinician and the individual agree to (Standard 2). The individual with OA must be reassessed, as needed, to understand the efficacy and side effects of the pharmacological treatment(s), and to highlight any need for modifications in a timely manner.
The algorithm should be read top to bottom. These tables provide example medications for each category from the algorithm.
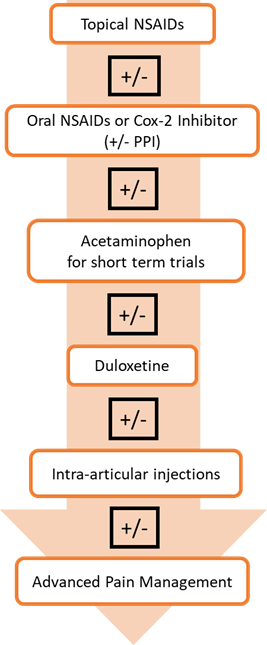
The algorithm begins with topical nonsteroidal anti-inflammatory drugs (NSAIDs) for individuals who have mild pain from their OA. Topical NSAIDs are better suited for knee OA versus the hip as the knee joint is closer to the surface of the skin allowing for better penetration of the medication. Next, consider an oral NSAIDs or Cox-2 inhibitor for patients without contraindications. NSAIDs and Cox-2 Inhibitors can cause serious side effects and increase risk of CV events. Try to use at the lowest dose for the shortest time-period possible. Consider providing a prescription for a PPI for gastroprotection in patients with increased GI risk. A short-term trial of acetaminophen could also be tried. Note that in clinical trials, acetaminophen appears to offer little clinically meaningful benefit. However, a short-term trial is often recommended as it is considered relatively safe compared to alternatives. This might also be a good choice for patients unable to take oral NSAIDs.
If oral NSAIDs do not provide adequate relief or a patient has a contraindication to oral NSAIDs, consider a trial of duloxetine for those with moderate to severe pain. Duloxetine has an official indication only for knee OA but may also be beneficial in patients with hip OA with comorbid depression and anxiety.
Intra-articular injections include: steroids, hyaluronic acid preparations and platelet rich plasma (PRP). These can be considered if complementary supplements are still not providing adequate pain relief. Stem cell therapy is also a form of intra-articular injection, but Health Canada has a moratorium on this therapy. Note: the evidence on all intra-articular injections is evolving and costs vs. benefits should be carefully considered.
The final option in the algorithm is advanced pain management. Advanced pain management includes:
- Opioids: oral or transdermal (not recommended)
- Peripheral nerve block
- Referral to an orthopaedic surgeon for joint surgery assessment (Standard 8)
Opioids are not recommended for routine use to treat OA pain88Ivers N, Dhalla IA, Allan GM. Opioids for osteoarthritis pain: Benefits and risks. Canadian Family Physician. 2012;58(12).. Opioids can have harmful side effects.
Cannabinoids are not routinely recommended for individuals with OA99Toward Optimized Practice (TOP). PEER simplified guideline: Medical Cannabinoids clinical practice guideline. 2018. .
PRESCRIBING ADJUNCT TREATMENTS
Pain medications must be prescribed very carefully, and a full history of the individual’s active prescriptions, history of addictions, comorbidities and pain experience must be evaluated. Based on the pharmaceutical treatment algorithm, develop a tailored medication plan taking into consideration the individual’s symptoms, ability to participate in Core Treatments, other health conditions, and values and preferences.
Use the Resource Inventory to track which Adjunct Treatments are available locally. Use the Tables of Examples of Conservative OA Treatments to consider the breadth of options for adjunct treatments.
Standard 3 describes how it is every clinician’s responsibility to communicate to the Primary Clinician, and vice versa. Any changes in the care plan or health status of the individual should be communicated. This is particularly important for the management of pharmacological treatments. Communications between clinicians can emphasize that the goal is to provide Adjunct Treatments to encourage return to Core Treatments.
At all follow-up visits, work with your individual with OA to reassess, track, and modify their Adjunct Treatments to better reflect their current needs and progress. This collaborative process will improve commitment to Core Treatments.
INTRODUCTION
Core Treatments (Standard 4, Standard 5, and Standard 6) are essential foundations of every care plan and have the strongest evidence for conservative management of osteoarthritis (OA)1-4. However, Adjunct Treatments can be considered if individuals with OA:
1Bowden JL, Hunter DJ, Deveza LA, Duong V, Dziedzic KS, Allen KD, et al. Core and adjunctive interventions for osteoarthritis: Efficacy and models for implementation. Nature Reviews Rheumatology. 2020;16(8):434-47.
2Gay C, Chabaud A, Guilley E, Coudeyre E. Educating patients about the benefits of physical activity and exercise for their hip and knee osteoarthritis. Systematic literature review. Annals of Physical and Rehabilitation Medicine. 2016;59(3):174-83.
3Rice D, McNair P, Huysmans E, Letzen J, Finan P. Best evidence rehabilitation for chronic pain part 5: Osteoarthritis. Journal of Clinical Medicine. 2019;8(11):1769.
4Wellsandt E, Golightly Y. Exercise in the management of knee and hip osteoarthritis. Current Opinion in Rheumatology. 2018;30(2):151-9.
- Find it difficult to participate in Core Treatments
- Report minimal progression toward their goals or
- Require additional support to manage symptoms
Adjunct Treatments are used to improve the individual’s ability to fully participate in Core Treatments. The clinician can provide evidence informed non-pharmacological and pharmacological treatments options to support the individual’s goals. In particular, muscle weakness, joint pain and fear of exacerbating symptoms can be barriers to adhering with prescribed exercise and physical activity (Standard 5). Addressing these physical and emotional barriers with Adjunct Treatments can support:
- Affected joints to ease mobility55Yu SP, Hunter DJ. Managing osteoarthritis. Australian Prescriber. 2015;38(4):115-9.
- Behavioural change11Bowden JL, Hunter DJ, Deveza LA, Duong V, Dziedzic KS, Allen KD, et al. Core and adjunctive interventions for osteoarthritis: Efficacy and models for implementation. Nature Reviews Rheumatology. 2020;16(8):434-47.
- Long-term commitment to exercise and physical activity11Bowden JL, Hunter DJ, Deveza LA, Duong V, Dziedzic KS, Allen KD, et al. Core and adjunctive interventions for osteoarthritis: Efficacy and models for implementation. Nature Reviews Rheumatology. 2020;16(8):434-47.
The clinician may refer to other disciplines with additional skills in OA management and expertise in specific Adjunct Treatments to build and strengthen the individual’s support network. This multidisciplinary care team approach combined with collaboration with the individual will ensure the individual’s priorities, values and preferences are considered when pursuing Adjunct Treatments. Any additional costs of Adjunct Treatments should be considered and discussed with the individual before adding to an OA care plan.
WALKING & ENVIRONMENTAL SUPPORTS
- Supports (walking and environmental)1,51Bowden JL, Hunter DJ, Deveza LA, Duong V, Dziedzic KS, Allen KD, et al. Core and adjunctive interventions for osteoarthritis: Efficacy and models for implementation. Nature Reviews Rheumatology. 2020;16(8):434-47.
5Yu SP, Hunter DJ. Managing osteoarthritis. Australian Prescriber. 2015;38(4):115-9. - Cognitive behavioural therapy11Bowden JL, Hunter DJ, Deveza LA, Duong V, Dziedzic KS, Allen KD, et al. Core and adjunctive interventions for osteoarthritis: Efficacy and models for implementation. Nature Reviews Rheumatology. 2020;16(8):434-47./span>
- Inter-disciplinary self-management programs11Bowden JL, Hunter DJ, Deveza LA, Duong V, Dziedzic KS, Allen KD, et al. Core and adjunctive interventions for osteoarthritis: Efficacy and models for implementation. Nature Reviews Rheumatology. 2020;16(8):434-47.
The use of walking supports can improve stability, mobilization, minimize the risk of falling and the severity of injury if a fall does occur, and reduce the lower limb loading that can increase pain. Walking supports include:
| Type | Facts and Benefits | Examples |
|---|---|---|
| Assistive Devices |
|
|
| Braces |
|
|
| Footwear and Orthotics |
|
Note: consider cost vs. benefit. See learn mores for more information. |
The use of environmental supports can conserve energy and provide options for safe movement. Environmental supports include:
| Type | Facts and Benefits | Examples |
|---|---|---|
| Assistive Technologies |
|
|
| Home Adaptations |
|
|
Supports are relatively affordable options that can address symptoms and allow individuals to better participate in exercise and physical activities. If these treatment options are applicable, the Primary Clinician can refer the individual to appropriate supporting clinicians or medical supply stores that are familiar with the walking supports commonly used by people with hip or knee OA. The individual can also self-refer to many clinicians who have supports expertise.
COGNITIVE BEHAVIOURAL THERAPY
COGNITIVE BEHAVIOURAL THERAPY11Bowden JL, Hunter DJ, Deveza LA, Duong V, Dziedzic KS, Allen KD, et al. Core and adjunctive interventions for osteoarthritis: Efficacy and models for implementation. Nature Reviews Rheumatology. 2020;16(8):434-47.
The individual’s OA pain experience can be influenced by changes in physical, emotional, behavioural, and cognitive states .
Cognitive behaviour therapy can be offered to individuals to:
- Support mental health
- Develop pain coping strategies
- Develop stress and anxiety management strategies
- Promote behavioural modifications
The clinician may offer advice for these or refer the individual to skilled supporting clinicians or other trained cognitive specialists.
SELF MANAGEMENT
Empowering individuals to play an active role in identifying what needs to change and set realistic goals including appropriate pace setting.
Helping individuals monitor their progression and changes in symptoms, in order to recognize when they need to ask for additional support.
Evaluation of progress in meeting goals and how to overcome barriers and challenges.
Guidance for managing emotional impacts of OA for individuals and their family support systems.
- Thermotherapy: Heat modalities and cryotherapy to manage joint inflammation; and
- Activity self-selection: Building their understanding of their local structured exercise programs and physical activity options so they can choose new ones as they wish.
When these programs are offered in a group setting, they can also provide an opportunity for individuals to build a support network, and feel less alone (universality). Peer support can improve self-management of OA6,76Ali SA, Walsh KE, Kloseck M. Patient perspectives on improving osteoarthritis management in urban and rural communities. Journal of pain research. 2018;11:417-25.
7Bryk C, Lewis TR, Miller J, Penman C, Teare S. The Experience of Waiting for Help with Osteoarthritis. Calgary, AB: PACER; 2013. Contract No.: Report. .
All education resources and sessions (Standard 4) will be combined with guidance on self-management strategies. The clinician should work with the individual to review and modify self-management strategies on an ongoing basis and as symptoms evolve.
PHARMACOLOGICAL INTERVENTIONS
- Non-prescription treatments: topical and oral
- Prescription treatments: topical and oral
- Intra-articular injectables
Pharmacological pain management strategies can be recommended by a primary care physician and/or in collaboration with a pharmacist or nurse practitioner. Prior to making pharmacological treatment recommendations, it is important that the clinician team assess the individual’s:
- Symptoms
- Pain experience
- Comorbidities
- History of pharmacological treatment use
Complications, side effects and possible interactions of the OA with other medicines should also be considered. Further consultation with other medical specialties may be required to ensure safety of the individual with OA prior to making recommendations. Intra-articular injections should be performed by a skilled clinician.
Symptom self-management strategies should be discussed in conjunction with pharmacological treatment planning. Pharmacological treatments should be used to reduce pain symptoms to promote and enable full participation in Core Treatments. Since medications cannot reduce pain to zero and come with the potential for side effects or tolerance development, encourage the individual to combine pharmacological treatments with other non-pharmacological treatments such as thermotherapy or activity self-selection to help optimize pain management.
As symptoms evolve, the pain management strategy must be modified to suit the individual’s current needs. Below is a stepped algorithm for pharmacological treatments that may be used by the clinician when considering options for best relief of the individual’s current pain symptoms. The individual’s needs, preferences, values, blood pressure, risks of side-effects and socio-economic status must be discussed when making pharmacological treatment choices. Selection of pharmacological treatments will influence the follow-up plan the clinician and the individual agree to (Standard 2). The individual with OA must be reassessed, as needed, to understand the efficacy and side effects of the pharmacological treatment(s), and to highlight any need for modifications in a timely manner.
The algorithm should be read top to bottom. These tables provide example medications for each category from the algorithm.
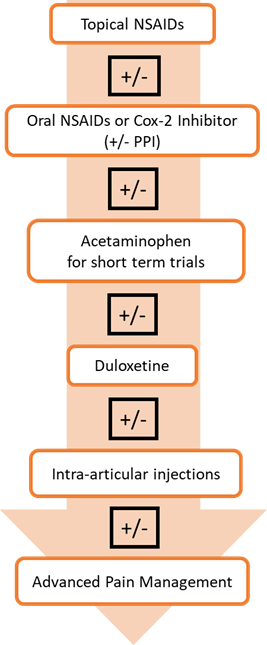
The algorithm begins with topical nonsteroidal anti-inflammatory drugs (NSAIDs) for individuals who have mild pain from their OA. Topical NSAIDs are better suited for knee OA versus the hip as the knee joint is closer to the surface of the skin allowing for better penetration of the medication. Next, consider an oral NSAIDs or Cox-2 inhibitor for patients without contraindications. NSAIDs and Cox-2 Inhibitors can cause serious side effects and increase risk of CV events. Try to use at the lowest dose for the shortest time-period possible. Consider providing a prescription for a PPI for gastroprotection in patients with increased GI risk. A short-term trial of acetaminophen could also be tried. Note that in clinical trials, acetaminophen appears to offer little clinically meaningful benefit. However, a short-term trial is often recommended as it is considered relatively safe compared to alternatives. This might also be a good choice for patients unable to take oral NSAIDs.
If oral NSAIDs do not provide adequate relief or a patient has a contraindication to oral NSAIDs, consider a trial of duloxetine for those with moderate to severe pain. Duloxetine has an official indication only for knee OA but may also be beneficial in patients with hip OA with comorbid depression and anxiety.
Intra-articular injections include: steroids, hyaluronic acid preparations and platelet rich plasma (PRP). These can be considered if complementary supplements are still not providing adequate pain relief. Stem cell therapy is also a form of intra-articular injection, but Health Canada has a moratorium on this therapy. Note: the evidence on all intra-articular injections is evolving and costs vs. benefits should be carefully considered.
The final option in the algorithm is advanced pain management. Advanced pain management includes:
- Opioids: oral or transdermal (not recommended)
- Peripheral nerve block
- Referral to an orthopaedic surgeon for joint surgery assessment (Standard 8)
Opioids are not recommended for routine use to treat OA pain88Ivers N, Dhalla IA, Allan GM. Opioids for osteoarthritis pain: Benefits and risks. Canadian Family Physician. 2012;58(12).. Opioids can have harmful side effects.
Cannabinoids are not routinely recommended for individuals with OA99Toward Optimized Practice (TOP). PEER simplified guideline: Medical Cannabinoids clinical practice guideline. 2018. .
PRESCRIBING ADJUNCT TREATMENTS
Use the Resource Inventory to track which Adjunct Treatments are available locally. Use the Tables of Examples of Conservative OA Treatments to consider the breadth of options for adjunct treatments.
Standard 3 describes how it is every clinician’s responsibility to communicate to the Primary Clinician, and vice versa. Any changes in the care plan or health status of the individual should be communicated. This is particularly important for the management of pharmacological treatments. Communications between clinicians can emphasize that the goal is to provide Adjunct Treatments to encourage return to Core Treatments.
At all follow-up visits, work with your individual with OA to reassess, track, and modify their Adjunct Treatments to better reflect their current needs and progress. This collaborative process will improve commitment to Core Treatments.
Custom Braces
Most osteoarthritis (OA) clinical guidelines do not cite strong evidence for braces for OA treatment, and therefore the guidelines do not recommend them. However, for some patterns of joint wear, some people with arthritis may find braces assist with pain management and foster a sense of confidence to continue with their exercise and physical activity.
Custom braces are more expensive than off-the-shelf braces. There may be assistance available from the Alberta Aids to Daily Living to assist with the cost of bracing. Bracing is not ideal for everyone with OA and the individual with OA is encouraged to speak to his/her health care provider to determine if this may be an option to consider.
Custom Orthotics
Custom orthotics are more expensive than off-the-shelf orthotics. Orthotics are not ideal for everyone with arthritis and the individual with OA is encouraged to speak to his/her health care provider to determine if this may be an option to consider.
Custom Footwear
Custom footwear is one example of walking supports that may offer a sense of pain relief and increased comfort to the individual with osteoarthritis (OA). They are typically made from a mold of the individual’s unique foot shape to accommodate an unusual foot shape. Custom footwear offers good heel control and an adequate toe box.
Most of the OA clinical guidelines do not cite strong evidence for custom footwear for OA treatment, and therefore the guidelines do not recommend them. However, custom footwear can provide confidence to the individual to continue with their exercise and physical activity.
Custom footwear are more expensive than off-the-shelf footwear and may not be of any greater benefit than a shoe that fits the foot well, with enough room in the toe box, fits the heel well without slipping and supports the arch of the foot.
Advanced Pain Management
Opioids are not recommended for routine use to treat osteoarthritis (OA) pain. Opioids have harmful side effects, including:
- Cognitive effects
- Increased risk of falls
- Increase in pain symptoms (opioid hyperalgesia)
- Risk of tolerance that may lead to dose escalation
- Risk of addiction and
- Risk of overdose, particularly if used in combination with other prescribed medications, alcohol, and/or in the presence of other health conditions including sleep apnea.
Prior to prescribing opioids, assess all risks and the medical history of the individual carefully. If the individual with OA requires advanced pain management, the clinicians should aim to prescribe the lowest effective dose, ideally <50mg morphine equivalents per day, and for a short duration. The Canadian Opioid Prescribing Guideline can also be consulted to provide further guidance. A strong opioid prescription plan for the individual includes:
- A clear discussion of the benefits and risks of opioids
- Instructions on when and how to consume the medication
- Instructions on the duration of the prescription
- A plan for frequent follow-up with the prescriber to ensure that the medication is helping for pain and function and not causing adverse side effects
- A naloxone kit with each prescription if prescribing to individuals at risk, such as those who:
- Are receiving a high dose
- Have a complex medical history and
- Have comorbidities
- A clear discussion about how short-term opioid use is meant to support the continued participation in Core Treatments.
The clinician should diligently monitor changes in the individual’s function, adherence to prescribed dose and frequency and any adverse side effects, which may require a treatment modification.
Peripheral Nerve Blocks
The body of evidence for injection treatments for osteoarthritis (OA) is evolving. Many OA clinical guidelines do not provide conclusive recommendations because of this. However, some individuals with OA respond very well to injections and can use them to continue comfortably with their Core Treatments.
Peripheral nerve blocks can be used at the knee to provide pain relief from OA. The geniculate nerve wraps around the knee and provides sensation to the joint. With ultrasound guidance, this nerve can be isolated and local anaesthetic can be infiltrated around the nerve. If ‘freezing’ the nerve results in pain relief for a few hours, this is a good indication that a procedure termed a radiofrequency ablation (‘burning’) of the geniculate nerve will provide more lasting pain relief.
Genicular Nerve Radiofrequency Ablation for Chronic Knee Pain | Spine and Pain Management in Fairfax, VAThe radio-frequency ablation is a simple, 10-minute procedure where a probe is passed through a small needle onto the nerve. Radio-frequency electrical waves are applied to the probe which ablates the nerve making it unable carry signals to the brain to sense pain. When this technique is applied to a knee with OA, six-to-12 months of pain relief is anticipated.
There is a risk of hypoesthesia as an adverse event. Individuals with OA should be observed for stability, perhaps complete a TUG test, before they are discharged from the treatment session.
Bone and Joint Health SCN
Opioids are not recommended for routine use to treat osteoarthritis (OA) pain. Opioids have harmful side effects, including:
- Cognitive effects
- Increased risk of falls
- Increase in pain symptoms (opioid hyperalgesia)
- Risk of tolerance that may lead to dose escalation
- Risk of addiction and
- Risk of overdose, particularly if used in combination with other prescribed medications, alcohol, and/or in the presence of other health conditions including sleep apnea.
Prior to prescribing opioids, assess all risks and the medical history of the individual carefully. If the individual with OA requires advanced pain management, the clinicians should aim to prescribe the lowest effective dose, ideally <50mg morphine equivalents per day, and for a short duration. The Canadian Opioid Prescribing Guideline can also be consulted to provide further guidance. A strong opioid prescription plan for the individual includes:
- A clear discussion of the benefits and risks of opioids
- Instructions on when and how to consume the medication
- Instructions on the duration of the prescription
- A plan for frequent follow-up with the prescriber to ensure that the medication is helping for pain and function and not causing adverse side effects
- A naloxone kit with each prescription if prescribing to individuals at risk, such as those who:
- Are receiving a high dose
- Have a complex medical history and
- Have comorbidities
- A clear discussion about how short-term opioid use is meant to support the continued participation in Core Treatments.
The clinician should diligently monitor changes in the individual’s function, adherence to prescribed dose and frequency and any adverse side effects, which may require a treatment modification.
Cannabinoids
Health Canada has stated that “there is no scientifically defined dose of cannabis for any medical condition”. Health Canada has also advised that the scientific evidence support the safety and efficacy of cannabinoids for medical purposes is unfounded.
For further reading the following are available for the clinician:
Alberta Health Services (AHS) directory of resources: https://www.albertahealthservices.ca/info/Page15989.aspx
For the individual with osteoarthritis (OA): myHealth Alberta provides answers to many frequently asked questions.
Intra-articular Injections
The body of evidence for injection treatments for osteoarthritis (OA) is evolving. Many OA clinical guidelines do not provide conclusive recommendations because of this. However, some individuals with OA respond very well to injections and can use them to continue comfortably with their Core Treatments.
Different injections have different purposes, and for some individuals a combination of injections may be appropriate, and different compounds may be injected at different times:
- Steroid (i.e. cortisone) is a potent anti-inflammatory medication. Steroids generally works quickly and generally does not provide lasting benefits compared to hyaluronic acid and/or platelet rich plasma. Steroids provide moderate pain relief and restoration of function; they are also cost-effective. Steroids are conditionally recommended for acute (1-2 weeks) and short term (4-6 weeks) pain relief. Consider repetitive injections if effective, no more often than three-four months.
- Hyaluronic acid (HA) is a compound found in normal, healthy joint fluid. HA is diminished in arthritic knees. HA injections are best in an arthritic joint, i.e. one that is not swollen. HA effects generally are more long lasting compared to steroids, possibly providing benefit for six-twelve months. HA provide improved pain relief and restoration of function compared with placebo.
- Theoretically, to be most effective the HA preparation has to be high molecular weight and highly cross-linked.
- Common OA clinical practice guidelines has been published for use with knees only, however it has been used effectively for hips as well.
- Platelet rich plasma (PRP) is a form of biologic injection that is an emerging therapeutic treatment option. Preparation varies by clinic; there is no Health Canada approved product in this category.
- Combining HA and steroids for knee OA patients can provide significant improvement in pain outcomes and may provide a more rapid onset, and longer duration of action than either therapy alone. However, there are potential concerns regarding cartilage loss with regular injecting this combination of therapies. There is insufficient evidence to support other combinations of intra-articular injection therapy.
Only some clinicians are trained in accurate injection delivery. “The accuracy of intra-articular injections depends on the joint and on the skills of the practitioner, imaging may improve accuracy.”
Steroid, HA and PRP injections can also be given with or without local anaesthetic. The effects of local anaesthesia on the cartilage are an emerging body of evidence as well.
Stem Cell Therapy
Peripheral Nerve Blocks
The body of evidence for injection treatments for osteoarthritis (OA) is evolving. Many OA clinical guidelines do not provide conclusive recommendations because of this. However, some individuals with OA respond very well to injections and can use them to continue comfortably with their Core Treatments.
Peripheral nerve blocks can be used at the knee to provide pain relief from OA. The geniculate nerve wraps around the knee and provides sensation to the joint. With ultrasound guidance, this nerve can be isolated and local anaesthetic can be infiltrated around the nerve. If ‘freezing’ the nerve results in pain relief for a few hours, this is a good indication that a procedure termed a radiofrequency ablation (‘burning’) of the geniculate nerve will provide more lasting pain relief.
The radio-frequency ablation is a simple, 10-minute procedure where a probe is passed through a small needle onto the nerve. Radio-frequency electrical waves are applied to the probe which ablates the nerve making it unable to carry signals to the brain to sense pain. When this technique is applied to a knee with OA, six-to-12 months of pain relief is anticipated.
There is a risk of hypoesthesia as an adverse event. Individuals with OA should be observed for stability, perhaps complete a TUG test, before they are discharged from the treatment session.
Shared Decision Making
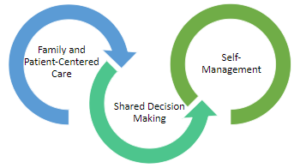
The inter-twining principles that ground the Comprehensive Quality Care Standards for Osteoarthritis of the Hip and Knee.
Shared decision-making (SDM) techniques and processes are emphasized throughout these standards. The use of SDM is essential to achieving ‘family and patient-centric’ care. SDM is evidence-based and proven to improve outcomes for the individual such as satisfaction with and adherence to care plans.
Standard 2 describes how sharing the decision making is important for building a care plan. This toolkit This toolkit provides more detail on the 3-talk model that can be used to practice SDM in everyday practice.
Alberta Referral Directory
Alberta Referral Directory to assist with:
- Identifying diagnostic imaging locations
- Orthopaedic surgery referral requirements to the Alberta Hip and Knee Program (if appropriate)
- Designing a local Resource Inventory and keeping it up to date
- Referral to other clinicians
Referral Between Clinicians
The following matrix is provided to guide clinicians on referrals and building a multi-disciplinary team of support for an individual with osteoarthritis (OA). Some supporting clinicians will work in a dedicated team at the same centre as a Primary Clinician, other supporting clinicians will work at separate organizations in the community.
| Category of OA Treatments | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Discipline that may offer the treatment | Education | Exercise and Physical Activity | Weight Management | Supports (Walking and Environmental | Cognitive Behavioural Therapy | Inter-disciplinary Self-Management Programs | Non-prescription Pharma Treatments | Prescription Pharma Treatments | Intra-articular Injections |
| Family Physicians | X | X* | X | X | X* | ||||
| Nurses | X | X | X | X* | |||||
| Physiotherapists | X | X | X | X* | X | Restricted | |||
| Occupational Therapists | X | X | X | X* | X | ||||
| Kinesiologists | X | X | X | ||||||
| Exercise Physiologists | X | X | X | ||||||
| Sport and Exercise Medicine Physicians | X | X | X | X | X | ||||
| Radiologists | X | ||||||||
| Rheumatologists | X | X | X | X | |||||
| Physiatrists | X | X | X | X | |||||
| Chiropractors | X | ||||||||
| Orthopaedic Surgeons | X | X | X | X | |||||
| Pharmacist | X | X | |||||||
| Registered Dietitians | X | X | |||||||
| Counsellors | X | X | X | ||||||
| Psychiatrists | X | X | X | ||||||
| Psychologists/Mental Health Therapists | X | X | X | ||||||
| Podiatrists | X | X | |||||||
| Pedorthists | X | ||||||||
Note: The method of delivery of conservative OA treatments can vary between disciplines, between practices and between communities. Clinicians should talk with their individual with OA to make sure the referral will be the right fit for the individual.*Note: Clinicians can offer these services with the applicable training.
Resource Inventory Notes
Resource Inventory Notes:
- Form clinic partnerships to create a common Resource Inventory for your local region
- Assign one person to review and update the Resource Inventory regularly
- Build relationships with the services listed on your Resource Inventory to make transition between care as smooth as possible for the individual with OA
- Keep accurate records of cost and wait times for local services to assist individuals wherever possible