STANDARD 3
Treatment selection will vary for each individual. To navigate a life-long journey with osteoarthritis (OA), it is important to strive for confidence in self-management. However, people with OA of the hip or knee often require support to manage this chronic and evolving condition. Tailoring treatments depends on the individual’s symptoms, experiences, needs, goals, and their care plan and self-efficacy. Collaboration between clinicians of different disciplines will likely be required as an individuals OA care journey develops.

OVERVIEW
- Every person’s life and OA symptoms evolve differently, their unique care plan should evolve with their needs and goals
- Repeated imaging is not required for ongoing tracking of OA, the individual’s clinical presentation and personal choices guides ongoing OA management
- Multi-disciplinary clinician collaboration is crucial for successful OA care
- If you are the Primary Clinician you take the lead in overseeing the care plan evolution over the individual’s lifetime and building a network of supporting clinicians (at the same clinic or separate organizations in the community)
- If you are a supporting clinician, you are responsible for clear communication back to the Primary Clinician, clear discharge planning, and warm hand overs
- Have a clear follow up plan established with the individual. Follow up to evaluate the response to a treatment, or to ‘check-in’ on OA evolution
- It can take over three months of dedication to most conservative treatments to see results
- The goal is to strive to empower, engage and educate the individual to self-manage their OA
KEY RESOURCES
- FORM to Track Trialled Treatments
- Shared Decision-Making Toolkit
- OA Self Management Toolkit
- SAMPLE Resource Inventory
- TEMPLATE Resource Inventory
- FORM to Document/Modify a Care Plan for Management of OA
- Tables of Examples for the Treatment Toolbox
- Health Change Methodology
- Alberta Referral Directory
TAILORING TREATMENTS
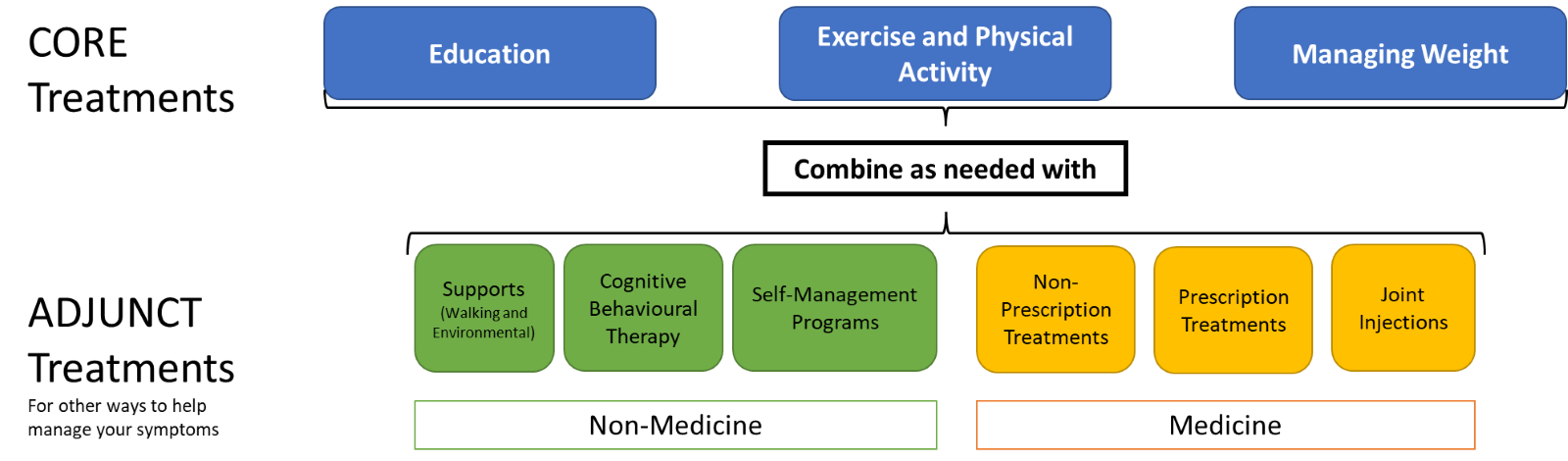
After starting the initial care plan (Standard 2), non-surgical osteoarthritis (OA) care will continue for everyone differently. This is because every person’s life and OA will evolve differently. Tailoring of care depends on symptom evolution, experience with treatments and individual needs.
As described in Standard 2, the non-surgical OA Treatments are used to build the initial care plan. The non-surgical OA Treatments can also be used to guide tailoring of the care plan as the individual’s symptoms and needs evolve. After building the initial care plan, it becomes a living document that should be modified and updated over the individual’s lifetime.
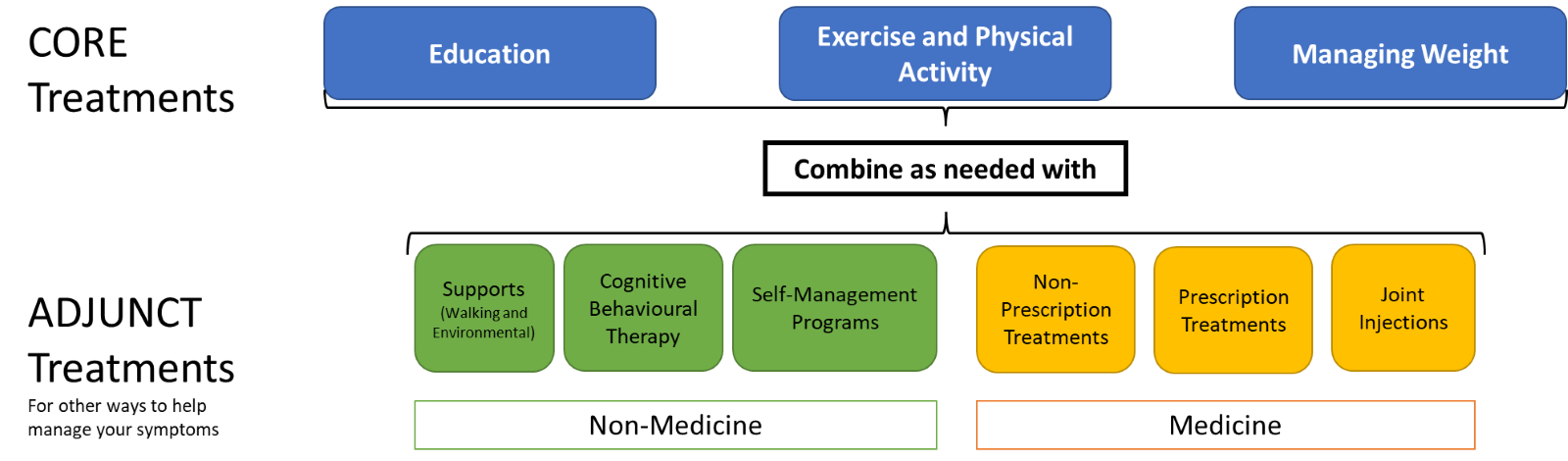
There are no one-size-fits-all rules for how to combine treatments and tailor care for the individual with OA; clinical expertise should be combined with the individual’s goals and needs. The care team will work with the person to determine if the selected treatments are effectively managing their symptoms and improving function to meet their goals. Treatments that were once effective may become ineffective for symptom management and/or the individual’s goals. Treatments that were ineffective may become effective again if they haven’t been trialed for some time.
Modifications are appropriate when the individual asks for them or if the clinician notices a decline in the individual’s function or quality of life. Shared decision-making techniques should be employed for conversations about care plan modification.
Standard 1 provides detail on how imaging is not required for OA diagnosis and does not reliably correlate with symptoms1. 1 Wang X, Oo WM, Linklater JM. What is the role of imaging in the clinical diagnosis of osteoarthritis and disease management? Rheumatology. 2018;57(suppl_4):iv51–iv60.
Imaging is also not necessary for ongoing monitoring of OA progression2. 2 Sakellariou G, Conaghan PG, Zhang W, Bijlsma JWJ, Boyesen P, D’Agostion MA, Dohert M, Fodor D, Kloppenburg M, Miese F, Naredo E, Porcheret M, Iagnocco A. EULAR recommendations for the use of imaging in the clinical management of peripheral joint osteoarthritis. Ann Rheum Dis. 2017 Sep;76(9):1484-1494. doi: 10.1136/annrheumdis-2016-210815. Epub 2017 Apr 7.
However, if symptoms progress rapidly and OA features need investigation then imaging can become important. Additionally, up to date imaging may be required to assist an orthopaedic surgeon in their surgery planning (Standard 8). A referral to a surgeon is a possible modification to a care plan but typically referral is not appropriate if at least 12 weeks of conservative treatment have not been trialed. The exception to this is if the criteria for immediate surgeon referral are met.
COLLABORATION
The clinician should work with the individual with OA to understand who the Primary Clinician for OA management is. It is beneficial when the Primary Clinician practices at the individual’s medical home and has prescribing privileges (i.e. for some Adjunct Treatments). It is through multi-disciplinary clinician collaboration, between the Primary Clinician and supporting disciplines, that the individual with OA will receive the best support for their care journey. Properly supported people are more likely to adopt treatment recommendations for a chronic and evolving condition like OA33Bowden JL, Hunter DJ, Deveza LA, Duong V, Dziedzic KS, Allen KD, et al. Core and adjunctive interventions for osteoarthritis: Efficacy and models for implementation. Nature Reviews Rheumatology. 2020;16(8):434-47..
The Primary Clinician should take the lead in:
- Building a network of supporting clinicians as the individual with OA trials different treatments
- Making introductions and seeking open communication (verbal or written) with the supporting clinicians to promote comprehensive and collaborative care for the individual
- Communicating the changes in the individual’s health status and care plan to the supporting clinicians as appropriate and
- Guiding the individual on modifying their care plan and tailoring their treatments over time
Many supporting clinicians will offer specific treatments for a structured period of time, rather than longitudinal care. Some supporting clinicians will work in a dedicated team at the same centre as a Primary Clinician, other supporting clinicians will work at separate organizations in the community. Supporting clinicians are responsible for:
- Asking the individual with OA to identify their Primary Clinician
- Seeking open communication (verbal or written) with the Primary Clinician throughout the treatment period, as required
- Planning and providing a clear discharge when appropriate and
- Providing a ‘warm hand over’ to the Primary Clinician after the treatment period
FOLLOW-UPS: PLANNING & EXECUTION
Education sessions can be delivered in verbal, written and/or virtual formats.
The purpose of follow-up appointments is to:
- Evaluate the response to a new treatment; and/or
- Monitor the evolution in symptomology and the need to modify a care plan
Similar to modifying the care plan, there is no one-size-fits-all for scheduling follow-ups. Regardless, the plan for follow-up should be clear between the individual and the clinician. Shared decision-making techniques should be used to structure the conversations about the follow-up plan and the individual with OA should be empowered to contact the clinician to change this plan whenever they have questions or a clinical concern. This form may be used to provide a record of the new follow-up plan when it is made.
Since OA is a chronic disease with no cure4, <sup4Hart DA, Werle J, Robert J, Kania-Richmond A. Long wait times for knee and hip total joint replacement in Canada: An isolated health system problem, or a symptom of a larger problem? Osteoarthritis and Cartilage Open. 2021;3(2):100141. the primary clinician will need to be in touch with the individual with OA for their lifetime. Frequency of follow-ups may vary with time, symptomology and needs of the individual. As the care plan evolves, the follow-up plan should evolve too.
SELF MANAGEMENT
The individual with OA lives with their disease every day, while clinicians, even the Primary Clinician, only briefly intersect with this journey. Throughout the OA journey, from building the initial care plan to end of life, the goal is to empower the individual to employ strategies to cope with their OA. Every Core Treatment (Standard 4, Standard 5, and Standard 6) emphasizes the principles of self-management, and Adjunct Treatment of Additional Self-Management Programs (Standard 7) provides an opportunity for more in-depth exploration of self-management techniques.
Individuals should be encouraged to record which OA treatments they have tried from the care plan and keep detailed notes on frequency, duration, changes in symptoms, and overall experience. Note: journaling can be accomplished in any format that is comfortable to the individual. Self-monitoring and evaluation should be encouraged during care planning and at follow-up visits, so individuals feel empowered and understand that they are in charge of their care journey.
Every clinician should support the individual to apply expanding OA knowledge to gain confidence in making treatment and self-management choices as symptoms change. Self-management coping strategies for OA include:
- Priority and goal setting
- Self-evaluation
- Problem-solving
- Mental health management
- Symptom management:
- Thermotherapies
- Activity self-selection
- Seeking clinician appointments as needed
TAILORING TREATMENTS
There are no one-size-fits-all rules for how to combine treatments and tailor care for the individual with OA; clinical expertise should be combined with the individual’s goals and needs. The care team will work with the person to determine if the selected treatments are effectively managing their symptoms and improving function to meet their goals. Treatments that were once effective may become ineffective for symptom management and/or the individual’s goals. Treatments that were ineffective may become effective again if they haven’t been trialed for some time.
Modifications are appropriate when the individual asks for them or if the clinician notices a decline in the individual’s function or quality of life. Shared decision-making techniques should be employed for conversations about care plan modification.
Standard 1 provides detail on how imaging is not required for OA diagnosis and does not reliably correlate with symptoms1. 1 Wang X, Oo WM, Linklater JM. What is the role of imaging in the clinical diagnosis of osteoarthritis and disease management? Rheumatology. 2018;57(suppl_4):iv51–iv60.
Imaging is also not necessary for ongoing monitoring of OA progression2. 2 Sakellariou G, Conaghan PG, Zhang W, Bijlsma JWJ, Boyesen P, D’Agostion MA, Dohert M, Fodor D, Kloppenburg M, Miese F, Naredo E, Porcheret M, Iagnocco A. EULAR recommendations for the use of imaging in the clinical management of peripheral joint osteoarthritis. Ann Rheum Dis. 2017 Sep;76(9):1484-1494. doi: 10.1136/annrheumdis-2016-210815. Epub 2017 Apr 7.
However, if symptoms progress rapidly and OA features need investigation then imaging can become important. Additionally, up to date imaging may be required to assist an orthopaedic surgeon in their surgery planning (Standard 8). A referral to a surgeon is a possible modification to a care plan but typically referral is not appropriate if at least 12 weeks of conservative treatment have not been trialed. The exception to this is if the criteria for immediate surgeon referral are met.
COLLABORATION
The Primary Clinician should take the lead in:
- Building a network of supporting clinicians as the individual with OA trials different treatments
- Making introductions and seeking open communication (verbal or written) with the supporting clinicians to promote comprehensive and collaborative care for the individual
- Communicating the changes in the individual’s health status and care plan to the supporting clinicians as appropriate and
- Guiding the individual on modifying their care plan and tailoring their treatments over time
Many supporting clinicians will offer specific treatments for a structured period of time, rather than longitudinal care. Some supporting clinicians will work in a dedicated team at the same centre as a Primary Clinician, other supporting clinicians will work at separate organizations in the community. Supporting clinicians are responsible for:
- Asking the individual with OA to identify their Primary Clinician
- Seeking open communication (verbal or written) with the Primary Clinician throughout the treatment period, as required
- Planning and providing a clear discharge when appropriate and
- Providing a ‘warm hand over’ to the Primary Clinician after the treatment period
FOLLOW-UPS: PLANNING & EXECUTION
The purpose of follow-up appointments is to:
- Evaluate the response to a new treatment; and/or
- Monitor the evolution in symptomology and the need to modify a care plan
Similar to modifying the care plan, there is no one-size-fits-all for scheduling follow-ups. Regardless, the plan for follow-up should be clear between the individual and the clinician. Shared decision-making techniques should be used to structure the conversations about the follow-up plan and the individual with OA should be empowered to contact the clinician to change this plan whenever they have questions or a clinical concern. This form may be used to provide a record of the new follow-up plan when it is made.
Since OA is a chronic disease with no cure4, <sup4Hart DA, Werle J, Robert J, Kania-Richmond A. Long wait times for knee and hip total joint replacement in Canada: An isolated health system problem, or a symptom of a larger problem? Osteoarthritis and Cartilage Open. 2021;3(2):100141. the primary clinician will need to be in touch with the individual with OA for their lifetime. Frequency of follow-ups may vary with time, symptomology and needs of the individual. As the care plan evolves, the follow-up plan should evolve too.
SELF MANAGEMENT
Individuals should be encouraged to record which OA treatments they have tried from the care plan and keep detailed notes on frequency, duration, changes in symptoms, and overall experience. Note: journaling can be accomplished in any format that is comfortable to the individual. Self-monitoring and evaluation should be encouraged during care planning and at follow-up visits, so individuals feel empowered and understand that they are in charge of their care journey.
Every clinician should support the individual to apply expanding OA knowledge to gain confidence in making treatment and self-management choices as symptoms change. Self-management coping strategies for OA include:
- Priority and goal setting
- Self-evaluation
- Problem-solving
- Mental health management
- Symptom management:
- Thermotherapies
- Activity self-selection
- Seeking clinician appointments as needed
Shared Decision Making
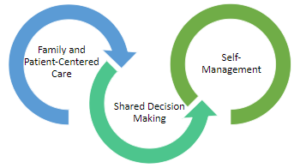
The inter-twining principles that ground the Comprehensive Quality Care Standards for Osteoarthritis of the Hip and Knee.
Shared decision-making (SDM) techniques and processes are emphasized throughout these standards. The use of SDM is essential to achieving ‘family and patient-centric’ care. SDM is evidence-based and proven to improve outcomes for the individual such as satisfaction with and adherence to care plans.
Standard 2 describes how sharing the decision making is important for building a care plan. This toolkit provides more detail on the 3-talk model that can be used to practice SDM in everyday practice.
Alberta Referral Directory
- Identifying diagnostic imaging locations
- Orthopaedic surgery referral requirements to the Alberta Hip and Knee Program (if appropriate)
- Designing a local Resource Inventory and keeping it up to date
- Referral to other clinicians
Resource Inventory Notes
- Form clinic partnerships to create a common Resource Inventory for your local region
- Assign one person to review and update the Resource Inventory regularly
- Build relationships with the services listed on your Resource Inventory to make transition between care as smooth as possible for the individual with OA
- Keep accurate records of cost and wait times for local services to assist individuals wherever possible
OA Self Management Toolkit
OA Self Management Toolkit, Includes:
Referral Between Clinicians
| Category of OA Treatments | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Discipline that may offer the treatment | Education | Exercise and Physical Activity | Weight Management | Supports (Walking and Environmental | Cognitive Behavioural Therapy | Inter-disciplinary Self-Management Programs | Non-prescription Pharma Treatments | Prescription Pharma Treatments | Intra-articular Injections |
| Family Physicians | X | X* | X | X | X* | ||||
| Nurse Practitioners | X | X | X | X* | |||||
| Physiotherapists | X | X | X | X* | X | Restricted | |||
| Occupational Therapists | X | X | X | X* | X | ||||
| Kinesiologists | X | X | X | ||||||
| Exercise Physiologists | X | X | X | ||||||
| Sport and Exercise Medicine Physicians | X | X | X | X | X | ||||
| Radiologists | X | ||||||||
| Rheumatologists | X | X | X | X | |||||
| Physiatrists | X | X | X | X | |||||
| Chiropractors | X | ||||||||
| Orthopaedic Surgeons | X | X | X | X | |||||
| Pharmacist | X | X | |||||||
| Registered Dietitians | X | X | |||||||
| Counsellors | X | X | X | ||||||
| Psychiatrists | X | X | X | ||||||
| Psychologists/Mental Health Therapists | X | X | X | ||||||
| Podiatrists | X | X | |||||||
| Pedorthists | X | ||||||||
Note: The method of delivery of conservative OA treatments can vary between disciplines, between practices and between communities. Clinicians should talk with their individual with OA to make sure the referral will be the right fit for the individual.
*Note: Clinicians can offer these services with the applicable training.
Warm Hand Over
There are a few reasons why a warm hand over may be required:
- A treatment with a supporting clinician is beginning
- A treatment with a supporting clinician is coming to an end
- A clinician reaches the limit of their scope of practice and the individual with osteoarthritis (OA) will require more advanced or different support and/or
- A new Primary Clinician is required
A warm hand over should include the following to achieve success:
- Discussion with the individual with OA to collaborate on:
- Understanding the need for a hand over and
- The selection of the new clinician
- Introductions between clinicians and with the individual with OA
- Chart sharing or transferring, as appropriate
- Discussion on next steps for support for the individual’s care plan and
- Review of the individual’s goals, values, preferences and needs
Scheduling Follow-ups
A follow-up to evaluate the response to a specific new treatment should be scheduled at a reasonable period to allow for the trial of the treatment. Clinical expertise or clinician consultation should be used to determine a reasonable trial period. Note that many active treatments require commitment and time to see results. However, the individual with osteoarthritis (OA) should be empowered to seek a follow-up prior to the scheduled appointment if any complications or concerns arise. Safe participation in the treatment is paramount, especially as the individual’s knowledge about OA treatments and confidence with self-management is evolving.
If the individual with OA is progressing well with treatments, it may simply be necessary to schedule a check-in at a reasonable period to ensure the overall wellbeing of the individual on their OA journey. There are several factors that may influence the scheduling of a follow-up appointment (see below). If you are the Primary Clinician, consider no more than one year between appointments. If you are a supporting clinician, collaborate with the Primary Clinician and the individual with OA to determine frequency of follow-ups. Regardless of the frequency period chosen for check-ins, the individual with OA should be empowered to seek appointments whenever they have concerns or questions.
The following factors may affect the overall frequency of follow-up appointments:
- The individual’s:
- Rate of symptom evolution and/or disease activity
- Quality of life changes
- Life circumstance changes (i.e. change in occupation or support)
- Socio-economic status
- Mental health
- Experience with other clinicians
- Physiological response to treatments and/or
- Preference for treatments
- A clinician’s:
- Practice preference and clinical expertise
- Clinic protocols
- Clinical expertise and/or
- Observations of the individual’s possible rate of disease activity
Modifying a Care Plan
To modify a care plan: review the documented and progression of health priorities, goals, values, preferences and overall wellbeing of the individual with osteoarthritis (OA). Document an updated assessment of the individual’s OA symptoms. Understand the experiences the individual had with previous treatments, such as:
- Physiological response to the treatment, especially if any complications or adverse reactions arose
- Preference for the treatment and/or
- Preference for the delivery mode of the treatment.
After the above information is reviewed and understood:
- Use the Tables of Examples of the OA Treatments Toolbox to suggest substitutions within categories or to suggest new treatments to build a new combination for the care plan, as appropriate.
- Discuss the importance of participating in Core Treatments
- Adjunct Treatment selections should support the continued participation in Core Treatments
- Final selections for care plan modification should be made through a collaboration between the individual and a clinician.
- The individual with OA can review their Treatment Menu to consider their interests in new treatments.
- Shared decision-making techniques can be used to guide this collaboration.
- Set new SMART goals for each new selection, keeping self-efficacy and new priorities in mind.
- Document changes to the care plan.
- Set a new follow-up plan
- Provide the individual with a copy of the modified care plan and the modified follow-up plan to promote self-management
- Communicate changes to the care plan to the full team of clinicians supporting the individual.
While the OA Treatments Toolbox is a tool for clinicians, the Treatment Menu and the Resource Inventory from the OA Self Management Toolkit are the individual-facing tools that align with the OA Treatments Toolbox.
The exception to the above guidelines is if referral to surgery is appropriate.
- Immediate referral to an orthopaedic surgeon may be appropriate if OA symptoms progress rapidly. Review the criteria for immediate referral to an orthopaedic surgeon.
- Referral to an orthopaedic surgeon may also be appropriate if non-surgical (conservative) treatments have been trialled and they are no longer effective (for symptom management and/or the individual’s goals).
- Refer to Standard 8 for details on referrals for joint surgery and continuation of OA management treatments during surgery wait times and after surgery. Hip or knee surgery is not the end of an OA care journey.
Discharge Planning
Discharge planning is crucial for treatments that have a scheduled end date (i.e. a 6-week structured pool therapy program). If discharge is applicable, supporting clinicians should introduce discharge planning at the beginning of a treatment to help prepare an individual with osteoarthritis (OA). Discharge planning should include:
- Acknowledging that the treatment will come to an end
- Discussing the intended outcomes of the treatment and the plans to measure these outcomes to demonstrate success of the treatment (Standard 9)
- Explaining what happens after the treatment
- i.e. Supporting clinician will write a letter back to the Primary Clinician.
- i.e. Individual will need to contact Primary Clinician to review and update or modify care plan.
- Providing examples of options if the treatment goals were not reached for the individual:
- i.e. Doing the treatment again
- i.e. Modifying the care plan to include:
- A different combination of treatments; or
- New, more intrusive and/or intensive treatments.
Supporting clinicians should seek opportunities to provide a warm hand over at the completion of discharge.
Scheduling Follow-ups
A follow-up to evaluate the response to a specific new treatment should be scheduled at a reasonable period to allow for the trial of the treatment. Clinical expertise or clinician consultation should be used to determine a reasonable trial period. Note that many active treatments require commitment and time to see results. However, the individual with osteoarthritis (OA) should be empowered to seek a follow-up prior to the scheduled appointment if any complications or concerns arise. Safe participation in the treatment is paramount, especially as the individual’s knowledge about OA treatments and confidence with self-management is evolving.
If the individual with OA is progressing well with treatments, it may simply be necessary to schedule a check-in at a reasonable period to ensure the overall wellbeing of the individual on their OA journey. There are several factors that may influence the scheduling of a follow-up appointment (see below). If you are the Primary Clinician, consider no more than one year between appointments. If you are a supporting clinician, collaborate with the Primary Clinician and the individual with OA to determine frequency of follow-ups. Regardless of the frequency period chosen for check-ins, the individual with OA should be empowered to seek appointments whenever they have concerns or questions.
The following factors may affect the overall frequency of follow-up appointments:
- The individual’s:
- Rate of symptom evolution and/or disease activity;
- Quality of life changes;
- Life circumstance changes (i.e. change in occupation or support);
- Socio-economic status;
- Mental health;
- Experience with other clinicians;
- Physiological response to treatments; and/or
- Preference for treatments.
- A clinician’s:
- Practice preference and clinical expertise;
- Clinic protocols;
- Clinical expertise; and/or
- Observations of the individual’s possible rate of disease activity.
Immediate or ‘Urgent’ Referral to Orthopaedic Surgeon
The goal with these standards is to encourage an adequate trial of non-surgical (conservative) OA treatment prior to referral to a surgeon (Standard 8). However, there are certain criteria that would result in an ‘urgent’ classification of the individual, and therefore warrant immediate referral to an orthopaedic surgeon. The individual’s experience is very important to consider as an arthroplasty has positive health outcomes for many individuals and can help them return to conservative OA management faster.
Refer immediately to an orthopaedic surgeon if:
- Other pathologies are identified:
- Suspected fracture or
- Ligament injury
- During the documenting of history or the performing of the physical exam the individual with OA describes all of the following:
- Dull/aching pain punctuated by short episodes of unpredictable pain and
- Pain interrupting sleep and
- Loss of independence and ability to do self care and
- Increase of frequency and dosing of pharmacological treatments and
- Avoidance of all daily activities.
- Increased reliance on use of narcotics
- Preliminary imaging was appropriately pursued and radiographical evidence reveals as severe joint spacing reduction.