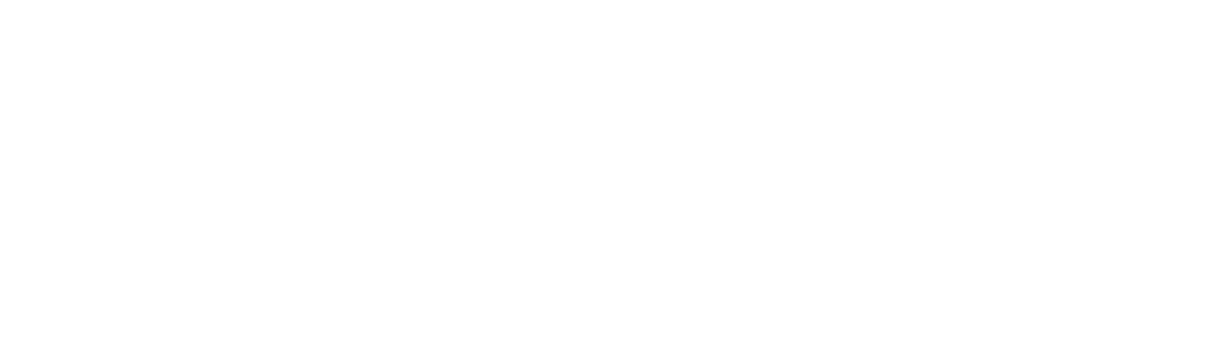
CORE TREATMENT 2 – EXERCISE AND PHYSICAL ACTIVITY
STANDARD 5
Exercise and physical activity programs are an important part of the care plan when you have OA of the hip or knee. Programs tailored for your needs offer support and information on progressive exercises and how to modify or change the activities as your symptoms change. These programs focus on improving your strength, endurance, and movement, which will help support regular movement and improve your overall health. Working with your clinician team will make sure your priorities, values, and preferences are part of setting exercise and physical activity goals.

OVERVIEW
- You might find that over time your legs are weaker,1,21de Zwart AH, Dekker J, Lems WF, Roorda LD, Van Der Esch M, Van Der Leeden M. Factors associated with upper leg muscle strength in knee osteoarthritis: A scoping review. Journal of rehabilitation medicine. 2018;50(2):140-50.
2Øiestad BE, Juhl CB, Eitzen I, Thorlund JB. Knee extensor muscle weakness is a risk factor for development of knee osteoarthritis. A systematic review and meta-analysis. Osteoarthritis and Cartilage. 2015;23(2):171-7. which may mean that you won’t be able to use or move them as well as before. - Not being active (sedentary) is one of the major risk factors of osteoarthritis, as it can make your symptoms worse, which can affect your quality of life33Musumeci G, Aiello FC, Szychlinska MA, Di Rosa M, Castrogiovanni P, Mobasheri A. Osteoarthritis in the XXIst century: Risk factors and behaviours that influence disease onset and progression. International Journal of Molecular Sciences. 2015;16(3):6093-112. and your overall health1-41de Zwart AH, Dekker J, Lems WF, Roorda LD, Van Der Esch M, Van Der Leeden M. Factors associated with upper leg muscle strength in knee osteoarthritis: A scoping review. Journal of rehabilitation medicine. 2018;50(2):140-50.
2Øiestad BE, Juhl CB, Eitzen I, Thorlund JB. Knee extensor muscle weakness is a risk factor for development of knee osteoarthritis. A systematic review and meta-analysis. Osteoarthritis and Cartilage. 2015;23(2):171-7.
3Musumeci G, Aiello FC, Szychlinska MA, Di Rosa M, Castrogiovanni P, Mobasheri A. Osteoarthritis in the XXIst century: Risk factors and behaviours that influence disease onset and progression. International Journal of Molecular Sciences. 2015;16(3):6093-112.
4Bowden JL, Hunter DJ, Deveza LA, Duong V, Dziedzic KS, Allen KD, et al. Core and adjunctive interventions for osteoarthritis: Efficacy and models for implementation. Nature Reviews Rheumatology. 2020;16(8):434-47.. - Regular exercise and physical activity are among the best treatments to improve your symptoms4,54Bowden JL, Hunter DJ, Deveza LA, Duong V, Dziedzic KS, Allen KD, et al. Core and adjunctive interventions for osteoarthritis: Efficacy and models for implementation. Nature Reviews Rheumatology. 2020;16(8):434-47.
5Rice D, McNair P, Huysmans E, Letzen J, Finan P. Best evidence rehabilitation for chronic pain part 5: Osteoarthritis. Journal of Clinical Medicine. 2019;8(11):1769. and maintain your overall wellness. - Most recommended exercises and physical activities for hip and knee OA focus on the lower half of your body (below the waist), including the trunk/core, gluteal, quadriceps, hamstring, and calf muscles
- Prescribed exercise can be done on your own or by joining a program. Over time and when it’s safe, you can gradually increase your daily physical activity by increasing how often, and how long you do the program.
KEY RESOURCES
- Finding Balance
- Glen Sather Sports Medicine Clinic Videos for Safe Exercises for Osteoarthritis
- Arthritis Society Flourish Exercise Videos
- Rehab Advice Line
- OA Self-Management Toolkit
- SAMPLE Resource Inventory
- FORM to Document/Modify a Care Plan for Conservative Management of OA
- MyHealth Alberta
- Healthier Together
- Arthritis Society Learning Modules
Speak with your clinician about strategies to manage your osteoarthritis along with the prescribed exercises that meet your needs and physical activity programs. Once you’re comfortable with your body and your options for modifying or changing your exercises and physical activities, you’ll be better able to safely exercise and do your day-to-day activities.
Prescribed Movement
During your care planning, your primary clinician should offer options for exercise and physical activity to focus on strength and flexibility and balancing it with your heart health. Or your primary clinician can refer you to other clinicians specialized in prescribed exercise to work with you to develop an exercise program.
Most recommended exercises and physical activities for hip and knee osteoarthritis focus on the lower half of your body (below the waist), including the trunk/core, gluteal, quadriceps, hamstring, and calf muscles. The muscles of the stomach and back help support the hips and knees.
It’s very common to be afraid that you’re going to hurt your joint even more or end up with an injury while exercising or doing your activities. However, your pain and stiffness aren’t directly related to the health of your joint.
It may feel confusing to be told you have to move a sore joint or body part, but exercise and moving a sore joint are important to keep joints healthy and slow the osteoarthritis. If you have other health conditions that could make activity risky for you, such as heart or lung conditions, make sure your clinicians know and work with them to safely modify your program.
A well-rounded movement plan4-64Bowden JL, Hunter DJ, Deveza LA, Duong V, Dziedzic KS, Allen KD, et al. Core and adjunctive interventions for osteoarthritis: Efficacy and models for implementation. Nature Reviews Rheumatology. 2020;16(8):434-47.
5Rice D, McNair P, Huysmans E, Letzen J, Finan P. Best evidence rehabilitation for chronic pain part 5: Osteoarthritis. Journal of Clinical Medicine. 2019;8(11):1769.
6Holden MA, Button K, Collins NJ, Henrotin Y, Hinman RS, Larsen JB, et al. Guidance for implementing best practice therapeutic exercise for people with knee and hip osteoarthritis: what does the current evidence base tell us? Arthritis Care & Research. 2020;Accepted for publication.:
- Accommodates for your baseline wellness
- Addresses your:
- Needs
- Goals
- Symptoms
- Budget limits
- Preferences
- Values
- Has an early plan for progression
- and incorporates:
- Daily movement goals (see below)
- Education on safe practices strategies for:
- Recovery
- Tracking and managing pain
- Pacing and modifying your activities
Note: Structured programs may cost money so talk with your clinician about what you’re able and willing to incorporate into your budget.
Physical Activity Target
8World Health Organization. WHO guidelines on physical activity and sedentary behavior. Geneva; 2020..
Description
You can carry a conversation while doing these activities
Examples
Brisk walking, biking, household chores, yard work, and dancing
Description
You’d feel a little out of breath during a conversation while doing these activities
Examples
Faster-paced walking, biking uphill, and swimming
Tips for Self-Managing Movement
- Start by measuring your ‘baseline’ pain
- Baseline pain is rating how strong your pain is while you’re sitting or resting and noting where it hurts
- Rate the pain between 0 and 10 (0 = no pain; 10 = the worst pain you can imagine) for each place where you feel it
- Do the recommended exercise or activity
- Once you’re done the exercise or activity, rate your pain and note the again where it hurts
If the pain goes back to baseline within 24 hours after you did the exercise or activity, keep doing them.
If your pain isn’t back to the baseline within 24 hours, the exercise or activity you did may have been too much for your joint.
Speak with your clinician team for advice on how to adjust the exercise and activity so that you do return to your baseline within 24 hours.
Referral Between Clinicians
| Category of OA Treatments | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Discipline that may offer the treatment | Education | Exercise and Physical Activity | Weight Management | Supports (Walking and Environmental | Cognitive Behavioural Therapy | Self-Management Programs | Non-prescription Pharma Treatments | Prescription Pharma Treatments | Joint Injections |
| Family Physicians | X | X* | X | X | X* | ||||
| Nurse Practitioners (NPs, RNs, LPNs) | X | X | X | X* | |||||
| Physiotherapists | X | X | X | X* | X | Restricted | |||
| Occupational Therapists | X | X | X | X* | X | ||||
| Kinesiologists | X | X | X | ||||||
| Exercise Physiologists | X | X | X | ||||||
| Sport and Exercise Medicine Physicians | X | X | X | X | X | ||||
| Radiologists | X | ||||||||
| Rheumatologists | X | X | X | X | |||||
| Physiatrists | X | X | X | X | |||||
| Chiropractors | X | ||||||||
| Orthopaedic Surgeons | X | X | X | X | |||||
| Pharmacist | X | X | |||||||
| Registered Dietitians | X | X | |||||||
| Counsellors | X | X | X | ||||||
| Psychiatrists | X | X | X | ||||||
| Psychologists/Mental Health Therapists | X | X | X | ||||||
| Podiatrists | X | X | |||||||
| Pedorthists | X | ||||||||
Managing Your OA
You understand that OA is a progressive disease with no cure. You live with your disease every day, while the clinicians provide support for short periods or short interactions. Throughout these 9 standards, the principles of self-management are reinforced. Confidence in self-management can be supported by the family and patient-centred care approach using SDM techniques.
All the processes and strategies described in these standards focus on supporting you as you learn more about your OA so you can have all the tools you need to make choices for your OA journey. The principles of self-management are vital to managing your symptoms day-to-day. Even when you’re doing everything ‘right’, OA can flare up for no reason that you can figure out. Once you understand this, and you have the tools you need, you’ll be ready to act when this happens.
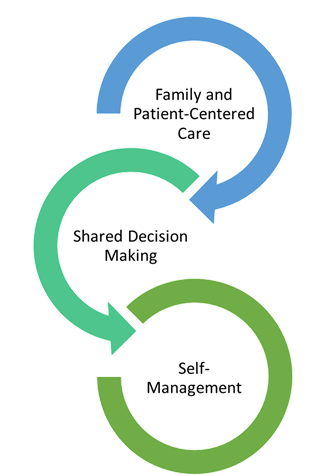
SDM
As care progresses, every clinician should support your treatment and coping choices. Other ways to manage your coping strategies for OA include:
- setting your priorities and goals
- managing your symptoms
- hot and cold therapies
- selecting your own activities
- manging your mental health
- making clinician appointments as needed
There’s more information in Standard 7 if you want to become even more confident in your self-management techniques.
OA SELF MANAGEMENT TOOLKIT
OA Self Management Toolkit, Includes: