ADJUNCT TREATMENTS
STANDARD 7
If you’re not able to try the Core Treatments, it’s taking longer than expected to reach your goals, or you need more support to manage symptoms, you can ask about Adjunct Treatments. They include non-medicine and medicine options to improve your pain, movement, and ability to take part in your Core Treatments. Working with your team to develop your Adjunct Treatment plan will ensure that your priorities, values, and preferences are considered when choosing them.

OVERVIEW
- Medicine will never make your OA pain go away. However, it usually helps reduce the pain about 30 to 50%.
- Your OA Self Management Toolkit has some examples of non-medicine and medicine Adjunct Treatments for you to talk to your clinician about.
- Opioids aren’t recommended to treat OA pain as they have serious health and safety risks.
- Health Canada hasn’t approved stem cell therapy for OA because there’s not enough evidence to prove that it’s safe.
- Cannabinoids aren’t usually used for OA because there’s not enough evidence to prove their safety.
Core Treatments are the basis of every care plan (Standard 4, Standard 5, and Standard 6). However, Adjunct Treatments can be considered if:
- You can’t try the Core Treatments
- It’s taking longer than it should to reach your goals
- You need more support to manage your symptoms
Adjunct Treatments are used to improve your ability to fully take part in your Core Treatments. The clinician can offer evidence-informed, non-medicine and medicine treatments options to support your goals. If you’re having a lot of pain, trouble doing the Core Treatments, and/or your symptoms aren’t being managed enough, talk to your clinician about Adjunct options. Muscle weakness, joint pain, and the fear of making symptoms worse can be barriers to doing the prescribed exercises and increasing your activity (Standard 5).
- Strategies to help you manage pain
- Improve the stability, strength, and mobility of your affected joint(s)55Yu SP, Hunter DJ. Managing osteoarthritis. Australian Prescriber. 2015;38(4):115-9.
- Lifestyle changes
- Your long-term commitment to exercise and physical activity11Bowden JL, Hunter DJ, Deveza LA, Duong V, Dziedzic KS, Allen KD, et al. Core and adjunctive interventions for osteoarthritis: Efficacy and models for implementation. Nature Reviews Rheumatology. 2020;16(8):434-47.

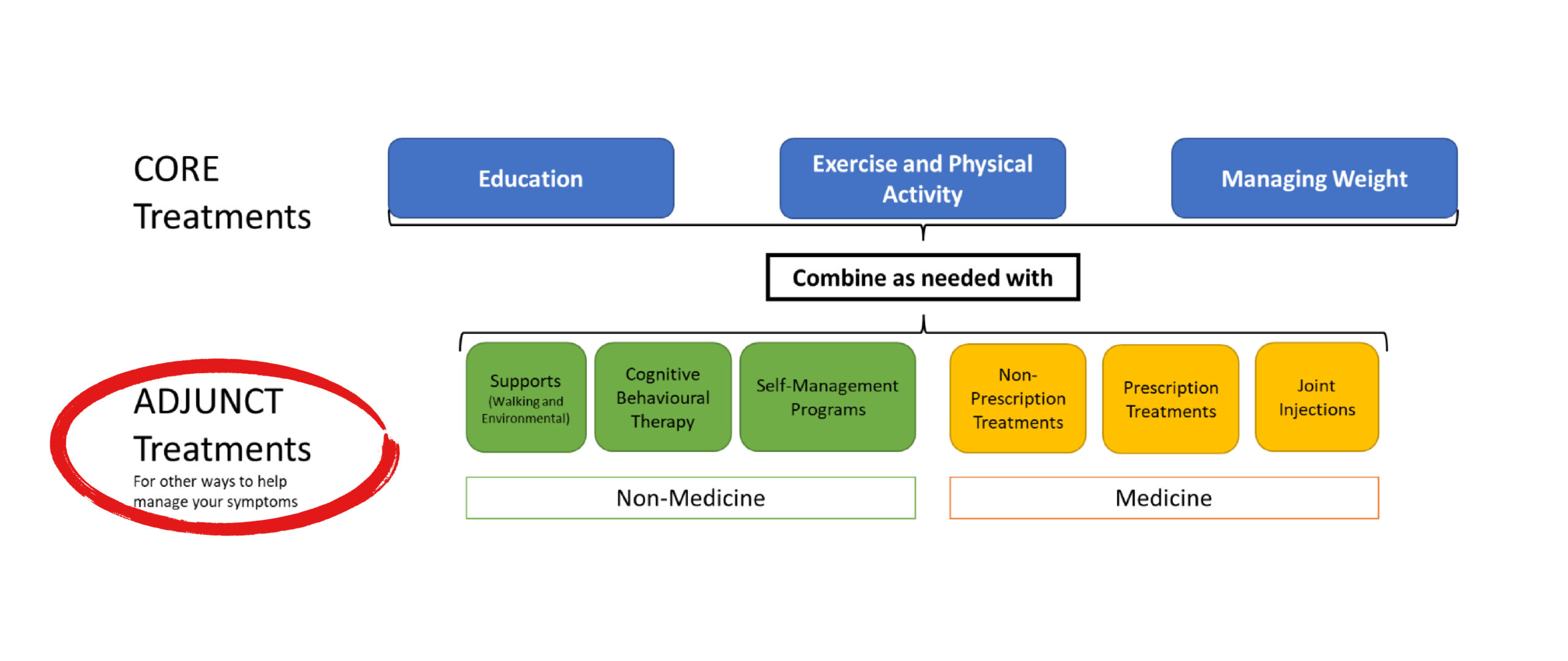
Non-Medicine Options
Non-Medicine options will help you address the physical and emotional barriers you face in your care journey. Medicine options may help you lower your pain to a level where you’re more comfortable. Talk to your clinician about what you prefer, and which options best suit your needs.
Non-medicine Adjunct Treatments include:
- Supports (walking and environmental)1,51Bowden JL, Hunter DJ, Deveza LA, Duong V, Dziedzic KS, Allen KD, et al. Core and adjunctive interventions for osteoarthritis: Efficacy and models for implementation. Nature Reviews Rheumatology. 2020;16(8):434-47.
5Yu SP, Hunter DJ. Managing osteoarthritis. Australian Prescriber. 2015;38(4):115-9. - Cognitive behavioural therapy (CBT)11Bowden JL, Hunter DJ, Deveza LA, Duong V, Dziedzic KS, Allen KD, et al. Core and adjunctive interventions for osteoarthritis: Efficacy and models for implementation. Nature Reviews Rheumatology. 2020;16(8):434-47.
- Self-management programs11Bowden JL, Hunter DJ, Deveza LA, Duong V, Dziedzic KS, Allen KD, et al. Core and adjunctive interventions for osteoarthritis: Efficacy and models for implementation. Nature Reviews Rheumatology. 2020;16(8):434-47.
Supports – Walking and Environmental
Using walking supports can improve your stability, how well you move, lower the risk of falling, and reduce the amount of weight on your hip or knee joint. The table below has examples of supports.
| Type | Facts and Benefits | Examples |
|---|---|---|
| Assistive Devices |
|
|
| Braces |
|
|
| Footwear and Orthotics |
|
|
Environmental supports can conserve energy and give you options for safe movement. They include the assistive technologies and home adaptions shown below.
| Type | What They Do | Examples |
|---|---|---|
| Items That Help You with Everyday Activities |
|
|
| Items That Can Help with Your Home Needs |
|
|
Supports can address symptoms and make it easier for you to do your exercise and physical activities. If there are treatment options that would work for you, your primary clinician can refer you to supporting clinicians or medical supply stores that know about the walking supports commonly used by people with hip or knee osteoarthritis. You can also refer yourself to many clinicians who have supports expertise. Supports are usually affordable. However, there may be some funding support so check with your insurance provider or ask your primary clinician if they know about any funding supports.
Cognitive Behavioural Therapy (CBT)
- Support your mental health11Bowden JL, Hunter DJ, Deveza LA, Duong V, Dziedzic KS, Allen KD, et al. Core and adjunctive interventions for osteoarthritis: Efficacy and models for implementation. Nature Reviews Rheumatology. 2020;16(8):434-47.
- Help you learn ways to cope with the pain11Bowden JL, Hunter DJ, Deveza LA, Duong V, Dziedzic KS, Allen KD, et al. Core and adjunctive interventions for osteoarthritis: Efficacy and models for implementation. Nature Reviews Rheumatology. 2020;16(8):434-47.
- Help you learn ways to manage your stress and anxiety11Bowden JL, Hunter DJ, Deveza LA, Duong V, Dziedzic KS, Allen KD, et al. Core and adjunctive interventions for osteoarthritis: Efficacy and models for implementation. Nature Reviews Rheumatology. 2020;16(8):434-47.
- Help you change your behaviour11Bowden JL, Hunter DJ, Deveza LA, Duong V, Dziedzic KS, Allen KD, et al. Core and adjunctive interventions for osteoarthritis: Efficacy and models for implementation. Nature Reviews Rheumatology. 2020;16(8):434-47.
Self-Management Programs
Self-management programs offer resources and strategies that can help support you. These programs focus on:
- Setting priorities and goals: Identify and set the SMART goals that are important to you
- Teaching you strategies to monitor your osteoarthritis so that you recognize when it’s time to ask for more support or help you keep working towards your goals
- Teaching you problem-solving strategies: To identify what may get in the way of you reaching your goals, and strategies for how to address them
- Teaching you strategies to cope with osteoarthritis: Give you the tools and guidance to manage the emotional impacts of osteoarthritis for you and your family support systems
- Teaching you ways to manage your symptoms
- Hot and cold therapies: Heat or cold can help relieve joint discomfort. Note: Don’t leave an ice pack on your skin for longer than 20 minutes at a time. The Osteoarthritis Self-Management Toolkit has more information about hot and cold therapies
- Selecting Your Activity: Building your understanding of your local structured exercise programs and physical activity options so you can choose new ones as you wish
When these programs are offered in a group setting, they also can help you meet others with osteoarthritis. Having the support of others on the osteoarthritis journey can improve how you manage your osteoarthritis.
All education resources and sessions will be combined with learning strategies to manage your osteoarthritis (Standard 4). The clinician will always work with you to review and modify your self-management strategies and as your symptoms change.
Medicine Options
There are 3 types of medications:
- Non-prescription
- Prescription
- Joint injections
Remember that medicine will never make all your OA pain go away. However, it can help reduce the pain 30% to 50%. That change in pain can help you continue with your Core Treatments, which will then help your osteoarthritis symptoms even more.
Medications can be recommended by a primary care physician and/or with a pharmacist or nurse practitioner. Before recommending medication it’s important that your clinician team assess:
- Your symptoms
- Your pain experience
- Other health issues you may have
- What other medicines you’ve taken
Complications, side effects, and possible ways the medication may work together are also considered. Your team will speak with other specialities as needed if there are questions about the medication you’re taking because of another health issue. Joint injections are only done by trained clinicians.
It’s important to talk about ways or strategies for you to manage your symptoms at the same time as planning for a new or different medication. Medicine won’t stop the pain. Some also have side effects, or your body builds up a tolerance to them, so combining medicine with other non-medicine treatments such as hot and cold therapies and the activities that you choose is the best strategy.
Your clinician will speak with you about all the benefits, risks, side effects, and how to best take the medicine. Make sure to take the medicine as directed and tell your clinician right away if you think you’re having side effects.
It’s also very important to tell your clinician if you have any changes in movement (function), pain, or other symptoms at all follow-up visits, so your medicine can be adjusted.
Other Therapies
Other therapies include joint injections, which include steroids, hyaluronic acid (HA) preparations, platelet rich plasma (PRP), and stem cells. Stem cell therapy for osteoarthritis isn’t allowed in Canada.
There are a few advanced options to help manage pain including:
- Peripheral nerve block
- Opioids
- Referral for a joint surgery assessment (Standard 8)
Opioids aren’t the first medication used to treat osteoarthritis pain88Ivers N, Dhalla IA, Allan GM. Opioids for osteoarthritis pain: Benefits and risks. Canadian Family Physician. 2012;58(12) because these drugs can have serious health and safety risks.
Cannabinoids have created great interest in people with osteoarthritis. Cannabinoids are compounds found in the cannabis plant (marijuana is a well-known example). However, cannabinoids aren’t usually recommended to treat osteoarthritis99Toward Optimized Practice (TOP). PEER simplified guideline: Medical Cannabinoids clinical practice guideline. 2018.. Health Canada maintains that there’s no scientific evidence that cannabinoids are safe and work for medical use. The topic Cannabinoids and Managing Chronic Pain from MyHealth.Alberta.ca answers many common questions about using cannabinoids.
Joint Injections
Many studies are being done looking at joint injections as a treatment for OA. The study results don’t tell us enough either way if joint injections should be a recommended treatment for OA. Because of this, the clinical guidelines can’t recommend them as a treatment. However, some people have responded well to injections so can keep using them alongside their Cores. Different injections have different purposes, and for some people a combination of injections may be a good choice for them:
- Steroid (e.g., cortisone) is a strong anti-inflammatory medication. Steroids generally work quickly and last for 1 to 6 months.
- Hyaluronic acid (HA) is a compound found in normal, healthy joint fluid. An arthritic joint has less HA in it. HA injections work best when the arthritic joint isn’t swollen. HA effects generally last 6 to 12 months.
- Platelet rich plasma (PRP) is a form of biologic injection that’s becoming used more as therapeutic treatment option. A small amount of your blood is withdrawn in a test tube and then spun in a machine. The blood cells fall to the bottom and the clear yellow fluid (the plasma) floats to the top. The plasma is then injected into the joint. Health Canada hasn’t approved PRP as a ‘drug’ treatment yet.
Only some clinicians are trained to give injections. Steroid, HA, and PRP treatments are given by sterile injection into the knee. This simple procedure can be done in your clinician’s office, or at a diagnostic imaging centre so the clinician can see the joint during the injection.
Only some clinicians are trained to give injections. Steroid, HA, and PRP treatments are given by sterile injection into the knee. This simple procedure can be done in your clinician’s office, or at a diagnostic imaging centre so the clinician can see the joint during the injection.
Advanced Pain Medication
Opioids
Opioids aren’t usually recommended to treat OA pain. Opioids can:
- affect your memory and concentration
- increase your risk of a fall
- increase your pain symptoms.
Opioids can also increase your risk of:
- building a tolerance, which means you need a higher dose to get the same effect.
- becoming addicted
- accidentally overdosing, especially if used with other prescription medicine like sleeping pills, or alcohol, or if you have other health issues like sleep apnea.
Before prescribing opioids, your clinician will assess all risks and your medical history carefully. If you do need advanced pain management, your clinicians will prescribe the lowest dose and for the shortest time. A strong opioid prescription plan includes:
- a talk about the benefits and risks of opioids
- a talk about how using opioids short-term is meant to support you during your core treatments
- instructions on when to use it, how to use it, and how long it’s for
- a follow-up to ensure it’s working and not causing side effects
- a naloxone kit with prescription (for some people).
Expect your clinician to closely watch for changes in your mobility and movement, that you’re taking the medication exactly as prescribed, and any side effects that may mean your medication needs to be adjusted.
Peripheral Nerve Blocks
This is like the ‘freezing’ used before a procedure, like stitching a wound or filling a cavity. In this case, the freezing is injected around a bundle of nerves. When the nerve is ‘frozen’, the brain doesn’t get pain messages from the nerves. If freezing the nerve(s) gives enough pain relief, a longer lasting solution may be an option.
If you lose sensation after a nerve block you may be at a higher risk for falls. In this case you may need a walking support after the treatment.
Referral Between Clinicians
| Category of OA Treatments | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Discipline that may offer the treatment | Education | Exercise and Physical Activity | Weight Management | Supports (Walking and Environmental | Cognitive Behavioural Therapy | Self-Management Programs | Non-prescription Pharma Treatments | Prescription Pharma Treatments | Joint Injections |
| Family Physicians | X | X* | X | X | X* | ||||
| Nurse Practitioners | X | X | X | X* | |||||
| Physiotherapists | X | X | X | X* | X | Restricted | |||
| Occupational Therapists | X | X | X | X* | X | ||||
| Kinesiologists | X | X | X | ||||||
| Exercise Physiologists | X | X | X | ||||||
| Sport and Exercise Medicine Physicians | X | X | X | X | X | ||||
| Radiologists | X | ||||||||
| Rheumatologists | X | X | X | X | |||||
| Physiatrists | X | X | X | X | |||||
| Chiropractors | X | ||||||||
| Orthopaedic Surgeons | X | X | X | X | |||||
| Pharmacist | X | X | |||||||
| Registered Dietitians | X | X | |||||||
| Counsellors | X | X | X | ||||||
| Psychiatrists | X | X | X | ||||||
| Psychologists/Mental Health Therapists | X | X | X | ||||||
| Podiatrists | X | X | |||||||
| Pedorthists | X | ||||||||
Smart Goals
| S | Specific | The goal is specific to the OA treatment selected (e.g., going to the pool for aerobics). |
| M | Measurable | How often you’ll do the activity (e.g., going to the pool 2 days a week). |
| A | Attainable | The goal is chosen in context of your life (e.g., going to the pool 2 days a week is an important but realistic change from what you’re doing now and a there’s a pool near you). |
| R | Rewarding | The goal is meaningful to you. (e.g., going to the pool includes a chance to visit with a close friend and you’ll be working on changes for your OA together). |
| T | Timely | The goal has some due dates (e.g., pool visits start next week, and you and your primary clinician will review them in 4 weeks) |
SMART goals take practice to write. They’re the most successful when you and your clinician create them together.
Stem Cells
Stem cells are cells that can change into any tissue in the body. In theory, stem cells can be changed into cartilage to replace the lost or damaged cartilage in an arthritic joint. Health Canada is studying using stem cells as a treatment so it can’t be used outside the study until more research is done into its safety.
Read more about Stem Cell Treatment for Osteoarthritis (MyHealthAlberta).