STANDARD 2

OVERVIEW
Key Messages for Development of a Care Plan
- A care plan is living document that describes the treatments discussed with the individual with OA and chosen to address their health concerns and goals
- Each care plan is tailored to the individual and should account for socio-economic status
- Using shared decision making techniques, select Core Treatments and combine with Adjunct Treatments as required to support full participation in the Core Treatments
- Attach SMART goals to the selected treatments
- Choose a specific review or follow up plan
KEY RESOURCES
INTRODUCTION
A care plan is a living document that describes the treatments discussed with the individual with OA and chosen to address their health concerns and goals. Each care plan is tailored to the individual and should account for their socio-economic status.
The conservative osteoarthritis (OA) care plan describes the treatments discussed with the individual and chosen to address a range of items. A care plan is a living document: it will evolve over time. Standard 3 describes how to tailor care over time after the initial care plan is created.
A care plan is developed considering the person’s:
- Assessed health concerns
- Readiness for change
- Goals
- Values and preferences
- Overall wellbeing and
- Prior experiences with OA conservative treatments
While keeping all the items described above in mind, an OA care plan will be built by:
- Selecting specific Core Treatment(s)
- If required: selecting a combination of specific Adjunct Treatment(s) to support participation in Core Treatments
- Attaching SMART goal(s) to the selected treatment(s) and
- Choosing a specific follow-up plan (Standard 3) and revising the care plan as necessary, based on the individual’s needs and preferences.
Building a Care Plan
Each individual seeks care at different points in their disease activity, their symptomology, and with varying levels of knowledge about OA.
The Conservative OA Treatments are provided below. They are structured to:
- Promote the trialling of Core Treatments,1-41Bowden JL, Hunter DJ, Deveza LA, Duong V, Dziedzic KS, Allen KD, et al. Core and adjunctive interventions for osteoarthritis: Efficacy and models for implementation. Nature Reviews Rheumatology. 2020;16(8):434-47.
2Gay C, Chabaud A, Guilley E, Coudeyre E. Educating patients about the benefits of physical activity and exercise for their hip and knee osteoarthritis. Systematic literature review. Annals of Physical and Rehabilitation Medicine. 2016;59(3):174-83.
3Rice D, McNair P, Huysmans E, Letzen J, Finan P. Best evidence rehabilitation for chronic pain part 5: Osteoarthritis. Journal of Clinical Medicine. 2019;8(11):1769.
4Wellsandt E, Golightly Y. Exercise in the management of knee and hip osteoarthritis. Current Opinion in Rheumatology. 2018;30(2):151-9. which have the strongest evidence for conservative OA management; and - Use Adjunct Treatments to support the return to these Core Treatments throughout a care journey
Core Treatments can be tailored to the individual’s needs and preferences. They include:
- Education11Bowden JL, Hunter DJ, Deveza LA, Duong V, Dziedzic KS, Allen KD, et al. Core and adjunctive interventions for osteoarthritis: Efficacy and models for implementation. Nature Reviews Rheumatology. 2020;16(8):434-47. to provide knowledge and skills that empower the individual with OA to understand the disease and available evidence-informed treatments – See Standard 4.
- Exercise and Physical Activity1,31Bowden JL, Hunter DJ, Deveza LA, Duong V, Dziedzic KS, Allen KD, et al. Core and adjunctive interventions for osteoarthritis: Efficacy and models for implementation. Nature Reviews Rheumatology. 2020;16(8):434-47.
3Rice D, McNair P, Huysmans E, Letzen J, Finan P. Best evidence rehabilitation for chronic pain part 5: Osteoarthritis. Journal of Clinical Medicine. 2019;8(11):1769. to encourage the individual to foster movement to influence joint health and achieve their activities of daily life – See Standard 5. - Weight Management1,31Bowden JL, Hunter DJ, Deveza LA, Duong V, Dziedzic KS, Allen KD, et al. Core and adjunctive interventions for osteoarthritis: Efficacy and models for implementation. Nature Reviews Rheumatology. 2020;16(8):434-47.
3Rice D, McNair P, Huysmans E, Letzen J, Finan P. Best evidence rehabilitation for chronic pain part 5: Osteoarthritis. Journal of Clinical Medicine. 2019;8(11):1769. to support the individual to prevent increased joint loading to influence joint health and achieve movement for their activities of daily life – See Standard 6.
Adjunct Treatments can also be tailored to the individual’s needs and preferences. They are used to support the trials of and achievement of Core Treatments. See Standard 7 for more information.
These tables provide examples of specific treatments in every treatment category to assist the clinician with the building of a care plan. More detail is available for clinician guidance on stepping through the conservative OA treatments toolbox. Shared decision-making techniques are evidence-based and promote satisfaction and success with the care plan.
The OA Self Management Toolkit is for individuals with OA. This document is an education booklet with introductory information about OA, and three tools for the individual: a Report Card, a Treatment Menu and an example Resource Inventory. These tools can support and empower the individual in choosing their own preferred treatment options and can promote self-management of conservative OA management in the long term.
It is important to keep in mind that each individual with OA seeks care at different points in their OA journey. Chronic disease management can be overwhelming to individuals with OA, particularly when individuals try to change too much at one time. For individuals that are ready, encourage them to start with setting one to two goals that are important to them, and breaking them down into smaller steps. Ultimately, the complexity of the care plan should be proportional to the individual’s experience and enthusiasm, while remaining realistic.
PUTTING A CARE PLAN INTO ACTION
As soon as feasible after an OA diagnosis, the individual with OA will have:
- A documented care plan
- Direction on actions to take to begin the care plan
- Begun trialling at least one treatment option and
- A plan for follow-up (more in Standard 3)
An example of how a multi-disciplinary team may be used to achieve an actioned care plan quickly is provided.
The exception to this is if the individual is a candidate for immediate referral to an orthopaedic surgeon (Standard 1). In which case a conservative treatment plan should still be created but in complement with the surgeon’s orders. Standard 8 talks more about how surgery may only be one step in the ongoing journey of conservative management of OA.
SMART GOALS
SMART goals are a tool of shared decision-making and are becoming more common in healthcare. The use of SMART goals can promote adherence to the non-surgical osteoarthritis (OA) management Care Plan by meeting the individual where they are at in their readiness to change. Meet the individual where they are at by tailoring the scope of the goal appropriately. This also helps both the individual and the clinician attach accountability to the changes. SMART goals are:
SMART goals take practice to write and are most successful when they are created in collaboration between a clinician and an individual with OA (shared decision-making). For some clinicians the skills required for the collaborative care described in these standards may be new territory. The following are suggestions for additional training that clinicians may find beneficial:
- This toolkit for learning more about shared decision-making techniques
- Health Change Methodology
- Motivational interviewing
- Any training that focuses on ‘family and patient centered care’
CONSERVATIVE OA TOOLBOX
To start the development of a care plan: understand the health priorities, goals, values, preferences, overall wellbeing and experiences with conservative treatments of your individual with osteoarthritis (OA) of the hip or knee. Use shared decision-making techniques with your individual to identify the most important problem to address and this will help guide the initial care recommendations you make.
Each individual seeks care at different points in their disease activity, their symptomology, and with varying levels of knowledge about OA. The Conservative OA Treatments should be tailored to the individual’s needs:
- Many individuals with OA will begin their journey early in their disease and can use the Conservative OA Treatments systematically, increasing the intensity and/or the intrusiveness of the treatments, as their disease progresses.
- Other individuals with OA will be seeking clinician support later in their disease progression and will immediately require a more complex care plan with a combination of Adjunct Treatments (Standard 7) to support some exploration of Core Treatments (Standard 4, Standard 5, and Standard 6).
For all individuals with OA, effective management requires trial and error with the evidence-based conservative treatments. Not all treatments will work for all individuals. Some treatments may work for a short period of time and then not again. Some treatments can be returned to after a long break and may be more successful when the individual’s goals, preferences or symptoms have changed.
The Conservative OA Treatments allow the clinician to use their expertise to combine any number of treatments to ultimately support:
- Ongoing engagement in Core Treatments; and
- Self-management
The following are instructions for how to use the Conservative OA Treatments to build a care plan. Also use these tables for specific examples of each sub-category of treatments.
- Choose Core Treatments first
- They have the strongest evidence for OA management.
- They should be emphasized every time a care plan is modified (Standard 3).
- Use Adjunct Treatments for additional symptom management
- The use of Adjunct Treatments enables the individual with OA to continue to participate in Core Treatments.
- Use clinical judgement to combine any treatments that will support the individual to participate in Core Treatments.
- Discuss with the individual the difference between the use of active treatments as opposed to passive treatments.
- Work with the individual with OA to set SMART goals for their selected treatment.
- Use your local Resource Inventory to discuss how and where the individual will trial the selected treatments.
- Document the care plan and discuss a specific plan for follow-up appointments (Standard 3).
- Provide the individual with a copy of the care plan and the follow-up plan to promote self-management
While the Conservative OA Treatments are a tool for clinicians, clinicians should not use it in isolation without collaborating with the individual. Shared decision-making techniques can be used to build the individual’s care plan. The Treatment Menu and the Resource Inventory from the OA Self Management Toolkit are the individual-facing tools that align with the Conservative OA Treatments.
Note: if the individual with OA presents with symptoms that require immediate referral to surgery (see Standard 1), then the building of a care plan should be structured to complement the orthopaedic surgeon’s orders, whether the individual is a surgical candidate or not. See Standard 8 for more details: the conservative OA management journey does not end with surgery.
INTRODUCTION
The conservative osteoarthritis (OA) care plan describes the treatments discussed with the individual and chosen to address a range of items. A care plan is a living document: it will evolve over time. Standard 3 describes how to tailor care over time after the initial care plan is created.
A care plan is developed considering the person’s:
- Assessed health concerns
- Readiness for change
- Goals
- Values and preferences
- Overall wellbeing and
- Prior experiences with OA conservative treatments
While keeping all the items described above in mind, an OA care plan will be built by:
- Selecting specific Core Treatment(s)
- If required: selecting a combination of specific Adjunct Treatment(s) to support participation in Core Treatments
- Attaching SMART goal(s) to the selected treatment(s) and
- Choosing a specific follow-up plan (Standard 3) and revising the care plan as necessary, based on the individual’s needs and preferences.
BUILDING A CARE PLAN
The Conservative OA Treatments are provided below. They are structured to:
- Promote the trialling of Core Treatments,1-41Bowden JL, Hunter DJ, Deveza LA, Duong V, Dziedzic KS, Allen KD, et al. Core and adjunctive interventions for osteoarthritis: Efficacy and models for implementation. Nature Reviews Rheumatology. 2020;16(8):434-47.
2Gay C, Chabaud A, Guilley E, Coudeyre E. Educating patients about the benefits of physical activity and exercise for their hip and knee osteoarthritis. Systematic literature review. Annals of Physical and Rehabilitation Medicine. 2016;59(3):174-83.
3Rice D, McNair P, Huysmans E, Letzen J, Finan P. Best evidence rehabilitation for chronic pain part 5: Osteoarthritis. Journal of Clinical Medicine. 2019;8(11):1769.
4Wellsandt E, Golightly Y. Exercise in the management of knee and hip osteoarthritis. Current Opinion in Rheumatology. 2018;30(2):151-9. which have the strongest evidence for conservative OA management; and - Use Adjunct Treatments to support the return to these Core Treatments throughout a care journey
Core Treatments can be tailored to the individual’s needs and preferences. They include:
- Education11Bowden JL, Hunter DJ, Deveza LA, Duong V, Dziedzic KS, Allen KD, et al. Core and adjunctive interventions for osteoarthritis: Efficacy and models for implementation. Nature Reviews Rheumatology. 2020;16(8):434-47. to provide knowledge and skills that empower the individual with OA to understand the disease and available evidence-informed treatments – See Standard 4.
- Exercise and Physical Activity1,31Bowden JL, Hunter DJ, Deveza LA, Duong V, Dziedzic KS, Allen KD, et al. Core and adjunctive interventions for osteoarthritis: Efficacy and models for implementation. Nature Reviews Rheumatology. 2020;16(8):434-47.
3Rice D, McNair P, Huysmans E, Letzen J, Finan P. Best evidence rehabilitation for chronic pain part 5: Osteoarthritis. Journal of Clinical Medicine. 2019;8(11):1769. to encourage the individual to foster movement to influence joint health and achieve their activities of daily life – See Standard 5. - Weight Management1,31Bowden JL, Hunter DJ, Deveza LA, Duong V, Dziedzic KS, Allen KD, et al. Core and adjunctive interventions for osteoarthritis: Efficacy and models for implementation. Nature Reviews Rheumatology. 2020;16(8):434-47.
3Rice D, McNair P, Huysmans E, Letzen J, Finan P. Best evidence rehabilitation for chronic pain part 5: Osteoarthritis. Journal of Clinical Medicine. 2019;8(11):1769. to support the individual to prevent increased joint loading to influence joint health and achieve movement for their activities of daily life – See Standard 6.
Adjunct Treatments can also be tailored to the individual’s needs and preferences. They are used to support the trials of and achievement of Core Treatments. See Standard 7 for more information.
These tables provide examples of specific treatments in every treatment category to assist the clinician with the building of a care plan. More detail is available for clinician guidance on stepping through the conservative OA treatments toolbox. Shared decision-making techniques are evidence-based and promote satisfaction and success with the care plan.
The OA Self Management Toolkit is for individuals with OA. This document is an education booklet with introductory information about OA, and three tools for the individual: a Report Card, a Treatment Menu and an example Resource Inventory. These tools can support and empower the individual in choosing their own preferred treatment options and can promote self-management of conservative OA management in the long term.
It is important to keep in mind that each individual with OA seeks care at different points in their OA journey. Chronic disease management can be overwhelming to individuals with OA, particularly when individuals try to change too much at one time. For individuals that are ready, encourage them to start with setting one to two goals that are important to them, and breaking them down into smaller steps. Ultimately, the complexity of the care plan should be proportional to the individual’s experience and enthusiasm, while remaining realistic.
PUTTING A CARE PLAN INTO ACTION
As soon as feasible after an OA diagnosis, the individual with OA will have:
- A documented care plan
- Direction on actions to take to begin the care plan
- Begun trialling at least one treatment option and
- A plan for follow-up (more in Standard 3)
An example of how a multi-disciplinary team may be used to achieve an actioned care plan quickly is provided.
The exception to this is if the individual is a candidate for immediate referral to an orthopaedic surgeon (Standard 1). In which case a conservative treatment plan should still be created but in complement with the surgeon’s orders. Standard 8 talks more about how surgery may only be one step in the ongoing journey of conservative management of OA.
SMART GOALS
SMART goals are a tool of shared decision-making and are becoming more common in healthcare. The use of SMART goals can promote adherence to the non-surgical osteoarthritis (OA) management Care Plan by meeting the individual where they are at in their readiness to change. Meet the individual where they are at by tailoring the scope of the goal appropriately. This also helps both the individual and the clinician attach accountability to the changes. SMART goals are:
SMART goals take practice to write and are most successful when they are created in collaboration between a clinician and an individual with OA (shared decision-making). For some clinicians the skills required for the collaborative care described in these standards may be new territory. The following are suggestions for additional training that clinicians may find beneficial:
- This toolkit for learning more about shared decision-making techniques
- Health Change Methodology
- Motivational interviewing
- Any training that focuses on ‘family and patient centered care’
CONSERVATIVE OA TOOLBOX
To start the development of a care plan: understand the health priorities, goals, values, preferences, overall wellbeing and experiences with conservative treatments of your individual with osteoarthritis (OA) of the hip or knee. Use shared decision-making techniques with your individual to identify the most important problem to address and this will help guide the initial care recommendations you make.
Each individual seeks care at different points in their disease activity, their symptomology, and with varying levels of knowledge about OA. The Conservative OA Treatments should be tailored to the individual’s needs:
- Many individuals with OA will begin their journey early in their disease and can use the Conservative OA Treatments systematically, increasing the intensity and/or the intrusiveness of the treatments, as their disease progresses.
- Other individuals with OA will be seeking clinician support later in their disease progression and will immediately require a more complex care plan with a combination of Adjunct Treatments (Standard 7) to support some exploration of Core Treatments (Standard 4, Standard 5, and Standard 6).
For all individuals with OA, effective management requires trial and error with the evidence-based conservative treatments. Not all treatments will work for all individuals. Some treatments may work for a short period of time and then not again. Some treatments can be returned to after a long break and may be more successful when the individual’s goals, preferences or symptoms have changed.
The Conservative OA Treatments allow the clinician to use their expertise to combine any number of treatments to ultimately support:
- Ongoing engagement in Core Treatments; and
- Self-management
The following are instructions for how to use the Conservative OA Treatments to build a care plan. Also use these tables for specific examples of each sub-category of treatments.
- Choose Core Treatments first
- They have the strongest evidence for OA management.
- They should be emphasized every time a care plan is modified (Standard 3).
- Use Adjunct Treatments for additional symptom management
- The use of Adjunct Treatments enables the individual with OA to continue to participate in Core Treatments.
- Use clinical judgement to combine any treatments that will support the individual to participate in Core Treatments.
- Discuss with the individual the difference between the use of active treatments as opposed to passive treatments.
- Work with the individual with OA to set SMART goals for their selected treatment.
- Use your local Resource Inventory to discuss how and where the individual will trial the selected treatments.
- Document the care plan and discuss a specific plan for follow-up appointments (Standard 3).
- Provide the individual with a copy of the care plan and the follow-up plan to promote self-management
While the Conservative OA Treatments are a tool for clinicians, clinicians should not use it in isolation without collaborating with the individual. Shared decision-making techniques can be used to build the individual’s care plan. The Treatment Menu and the Resource Inventory from the OA Self Management Toolkit are the individual-facing tools that align with the Conservative OA Treatments.
Note: if the individual with OA presents with symptoms that require immediate referral to surgery (see Standard 1), then the building of a care plan should be structured to complement the orthopaedic surgeon’s orders, whether the individual is a surgical candidate or not. See Standard 8 for more details: the conservative OA management journey does not end with surgery.
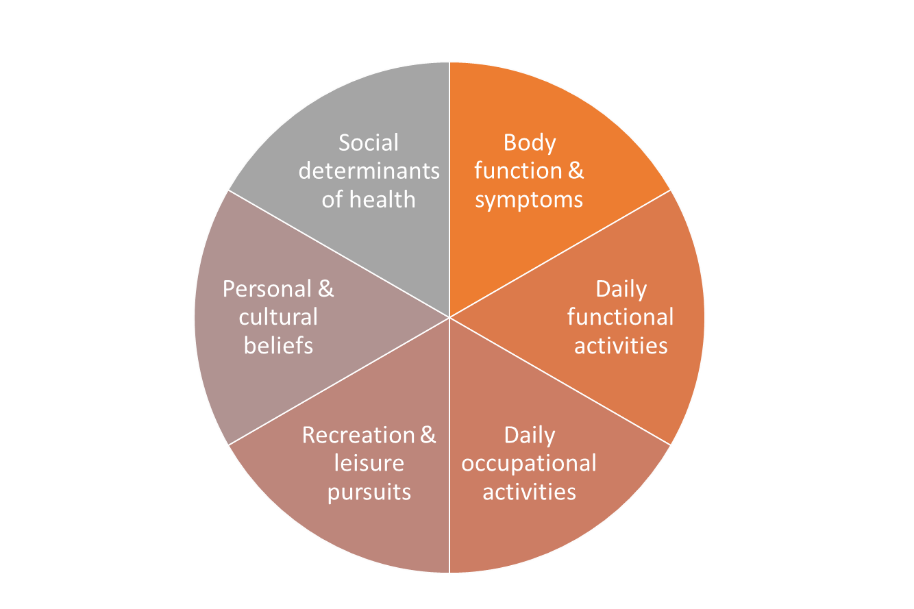
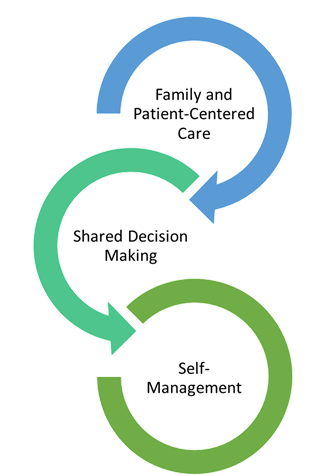
Shared Decision Making
The inter-twining principles that ground the Comprehensive Quality Care Standards for Osteoarthritis of the Hip and Knee.
Shared decision-making (SDM) techniques and processes are emphasized throughout these standards. The use of SDM is essential to achieving ‘family and patient-centric’ care. SDM is evidence-based and proven to improve outcomes for the individual such as satisfaction with and adherence to care plans.
Standard 2 describes how sharing the decision making is important for building a care plan. This toolkit This toolkit provides more detail on the 3-talk model that can be used to practice SDM in everyday practice.
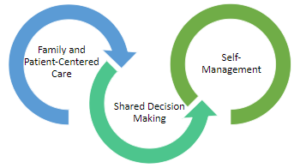
Overall Wellbeing
A conservative osteoarthritis (OA) management care plan considers the individual’s overall wellbeing. Overall wellbeing includes multiple factors:
- Body function and symptoms such as pain, swelling, joint range of motion, strength, balance, and any comorbidities.
- Mental health fitness.
- Daily functional activities such as personal care, walking, climbing stairs, sleep, housework, and meal preparation.
- Daily occupational activities such as employment and family responsibilities.
- Recreation and leisure pursuits and interests.
- Personal and cultural beliefs and attitudes towards health, activity, and exercise.
- Social determinants of health including socioeconomic status, education level, health literacy, family support systems, food and shelter security.
Elements of wholistic care planning.
Active versus Passive Treatments
The word ‘treatment’ is used to describe evidence-based options for conservative osteoarthritis (OA) management. Treatments can encompass a range of interactions between an individual and a clinician:
- Active treatments: the individual with OA is a full participant in the treatment (i.e. pool therapy program and using self-management skills).
- Passive treatments: the individual with OA receives an intervention from a clinician (i.e. an intra-articular injection).
Regardless of whether the treatment is active or passive, throughout these nine standards the principles of ‘family and patient centred' care are emphasized to encourage the use of shared decision-making techniques with the individual with OA and ultimately to promote self-management of OA.
Example of Appointment Structure: Diagnosis to Care Plan Start
Below is a template for appointment structuring, which clinicians/clinician teams might consider adopting to work in alignment with these standards. Collaboration between physicians and allied health strengthens the experience for an individual with osteoarthritis (OA) for these first few appointments. Identify the person in your team who is best suited and has the greatest strength or training for the activities described below. For instance: therapists (e.g. physiotherapists, occupational therapists) have extensive training in setting SMART goals using shared decision-making techniques.
- Individual presents with pains that may indicate OA.
- Schedule individual for comprehensive assessment appointment.
- Primary clinician of individual’s choice (See Standard 3)
- Comprehensive assessment. Confirm OA diagnosis.
- Primary clinician (who can diagnose OA)
- Introduce the OA Self Management Toolkit and provide it as a handout for home reading.
- Allied health
- Ask the individual to reflect on their goals and values to support the:
- SMART goal writing process and
- Treatment choosing process for the next visit.
- Allied health
- Explain Core vs. Adjunct Treatments.
- Consider using small group appointments to promote community building among individuals with OA
- Allied Health
- Collaborate to build a care plan
- Allied health
- Review and choose a follow-up plan
- Primary clinician
Alberta Referral Directory
Alberta Referral Directory to assist with:
- Identifying diagnostic imaging locations
- Orthopaedic surgery referral requirements to the Alberta Hip and Knee Program (if appropriate)
- Designing a local Resource Inventory and keeping it up to date
- Referral to other clinicians
OA Self Management Toolkit
OA Self Management Toolkit, Includes:
OA Self Management Toolkit, Includes:
Osteoarthritis Self Management Toolkit
The Osteoarthritis (OA) Self Management Toolkit is a handout for the individual with OA. It is evidence-based and adaptable to many healthcare settings. The toolkit can be used to build a care plan and to progress a care plan over time as the individual’s symptoms progress.
The OA Self Management Toolkit was designed with the principles of ‘family and patient-centric care’ in mind. The tools are easy to use in combination with shared decision making techniques to promote the individual’s self-management of their OA.It was also created in collaboration with individuals with OA.
| Tool in OA Self Management Toolkit Components | Purpose of the Component |
|---|---|
| Education Booklet | Provides introductory information on OA from basic facts to introductions to coping techniques. |
| Report Card | A one-time worksheet for the individual with OA to reflect on their experiences of OA treatments to date and identify their values and goals. |
| Treatment Menu |
Presents specific examples of treatment options for the individual with OA to select from. The menu is structured in alignment with strength of evidence for the treatment11Bowden JL, Hunter DJ, Deveza LA, Duong V, Dziedzic KS, Allen KD, et al. Core and adjunctive interventions for osteoarthritis: Efficacy and models for implementation. Nature Reviews Rheumatology. 2020;16(8):434-47. . The menu aligns with the OA Treatments Toolbox (Core Treatments are higher on the menu) but presents the treatments in a public facing way that promotes ongoing trial and error, and self-choice for the individual with OA. |
| Resource Inventory |
Aligned with the Treatment Menu structure, this tool presents specific information on ‘where’ and ‘how’ the individual with OA can trial their selected treatments. It is crucial to putting an OA management care plan into action. Resource Inventories are region specific and should be actively maintained for local accuracy. This is an Example of regionally adapted Resource Inventory. This is a Template for creating a new regionally adapted Resource Inventory. |
SMART Goals
SMART goals are a tool of shared decision-making and are becoming more common in healthcare. The use of SMART goals can promote adherence to the non-surgical osteoarthritis (OA) management Care Plan by meeting the individual where they are at in their readiness to change. Meet the individual where they are at by tailoring the scope of the goal appropriately. This also helps both the individual and the clinician attach accountability to the changes. SMART goals are:
SMART goals take practice to write and are most successful when they are created in collaboration between a clinician and an individual with OA (shared decision-making). For some clinicians the skills required for the collaborative care described in these standards may be new territory. The following are suggestions for additional training that clinicians may find beneficial:
- This toolkit for learning more about shared decision-making techniques
- Health Change Methodology
- Motivational interviewing
- Any training that focuses on ‘family and patient centered care’
Using the Osteoarthritis Treatments Toolbox
The following are instructions for how to use the Conservative OA Treatments Toolbox to build a care plan. Also use these tables for specific examples of each sub-category of treatments.
- Choose Core Treatments first
- They have the strongest evidence for OA management.
- They should be emphasized every time a care plan is modified (Standard 3).
- Use Adjunct Treatments for additional symptom management
- The use of Adjunct Treatments enables the individual with OA to continue to participate in Core Treatments.
- Use clinical judgement to combine any treatments that will support the individual to participate in Core Treatments.
- Discuss with the individual the difference between the use of active treatments as opposed to passive treatments .
- Work with the individual with OA to set SMART goals for their selected treatment.
- Use your local Resource Inventory to discuss how and where the individual will trial the selected treatments.
- Document the care plan and discuss a specific plan for follow-up appointments (Standard 3).
- Provide the individual with a copy of the care plan and the follow-up plan to promote self-management
While the Conservative OA Treatments Toolbox are a tool for clinicians, clinicians should not use it in isolation without collaborating with the individual. Shared decision-making techniques can be used to build the individual’s care plan. The Treatment Menu and the Resource Inventory from the OA Self Management Toolkit are the individual-facing tools that align with the Conservative OA Treatments Toolbox.
Note: if the individual with OA presents with symptoms that require immediate referral to surgery (see Standard 1), then the building of a care plan should be structured to complement the orthopaedic surgeon’s orders, whether the individual is a surgical candidate or not. See Standard 8 for more details: the conservative OA management journey does not end with surgery.
Self-Management
Osteoarthritis (OA) is a progressive disease with no cure. Osteoarthritis Research Society International (OARSI) and Patient and Community Engagement Research (PaCER) findings have concluded that the individual needs to have control of their care journey. The individual lives with their evolving disease every day, while the clinicians only provide support for short periods of time or short interactions1313Not available.. Throughout these nine standards, the principles of self-management are reinforced. Confidence in self-management can be supported by employing ‘family and patient-centred care’ principles using shared decision-making techniques.
All the processes and strategies described in these standards focus on empowering the individual to gain knowledge and to make choices for their OA journey based on that expanding knowledge. The principles of self-management are crucial to day-to-day symptom management. Symptoms of OA can flare up without explanation and the empowered, engaged and educated individual will be able to take action when this occurs.
As care progresses, every clinician should support the individual to gain confidence in applying their expanding OA knowledge to make treatment and self-management choices. Self-management strategies for OA include:
- Priority and goal setting
- Self-evaluation
- Problem-solving
- Mental health management
- Symptom management:
- Thermotherapies
- Activity self-selection
- Seeking clinician appointments as needed
More detail is provided in Standard 7 for those individuals who want to build more confidence in self-management techniques.
Regulated Health Care Professionals
- Family Physicians
- Nurse Practitioners
- Physiotherapists (Allied Health)
- Occupational Therapists (Allied Health)
- Pharmacists (Allied Health)
- Registered Dietitians (Allied Health)
- Psychiatrists
- Psychologists/Mental Health Therapists
- Chiropractors
- Specialty Physicians including:
- Sport and Exercise Medicine Physicians
- Radiologists
- Rheumatologists
- Physiatrists
- Orthopedic Surgeons
Osteoarthritis Clinicians
- Family physicians
- Nurse practitioners
- Physiotherapists
- Occupational therapists
- Specialty physicians including:
- Sport and exercise medicine physicians
- Rheumatologists
- Physiatrists
- Chiropractors
- Orthopedic surgeons
Regulated Health Care Professionals:
- Family physicians
- Nurse practitioners
- Physiotherapists (Allied Health)
- Occupational therapists (Allied Health)
- Pharmacists (Allied Health)
- Registered Dietitians (Allied Health)
- Psychiatrists
- Psychologists/mental health therapists
- Specialty physicians including:
- Sport and exercise medicine physicians
- Radiologists
- Rheumatologists
- Physiatrist
- Chiropractors
- Orthopedic surgeons
Non-regulated Health Care Professionals:
- Podiatrists
- Pedorthists
- Kinesiologists
- Exercise physiologists
- Recreational therapists
- Counsellors