STANDARD 1

OVERVIEW
Key Messages for Clinician Assessment
Adults (typically aged 40+) who present with joint pain, swelling or stiffness in hips, knees or lowers backs should be thoroughly examined for a diagnosis of OA.
- Screening questions, ruling out red flags and assessing for yellow flags
- Health history
- Physical exam
Imaging and laboratory investigations are not required to assist with clinical OA diagnosis of typical presentation. Findings on imaging may not always match the individual’s symptoms, and do not predict the response to treatment.
If required, weight bearing x-rays are the most appropriate imaging for viewing OA degradation.
Stay familiar with the criteria for immediate referral to an orthopaedic surgeon as every individual seeks care at a different stage of their journey.
The use of the terms ‘early’, ‘moderate/mild’ or ‘late/advanced’ are not recommended to describe clinical presentation of OA because they don’t accurately describe an individual’s lived experience.
INTRODUCTION
This standard sets out the components that should be present to make an accurate clinical diagnosis of osteoarthritis (OA). OA is a chronic disease caused by joint changes from a progression of cartilage loss which may result in pain, declining quality of life, loss of function and increasing disability.
Both regulated and non-regulated clinicians may be involved in the assessment and care of an individual with OA.
Adults (typically aged 40 years and older) who present with joint pain, swelling or stiffness in their hips, knees or lower backs should be assessed thoroughly to determine if they have OA in their knees or hips. 1, 2
1 Arthritis Association of Canada, The College of Family Physicians of Canada, Centre for Effective Practice. Osteoarthritis tool. 2017.
2 The Arthritis Society. Getting a grip on arthritis: Best practice guidelines. 2017.
Osteoarthritis of the hip or knee will likely present with at least one of these symptoms:
- Persistent atraumatic movement-related joint pain
- Aching
- Swelling
- Joint instability due to bone misalignment
- Catching
- Morning stiffness lasting less than 30 minutes
These symptoms may affect more than one joint at a time. Prior injuries, existing comorbidities and congenital deformities may be present along with typical OA symptoms.
If the individual does not have hip and/or knee OA or meets criteria for consideration for inflammatory arthritis then these standards are not appropriate and other guidelines and tools should be used to inform diagnoses and care.
SCREENING
If OA is suspected, a diagnosis can be made with a comprehensive biopsychosocial clinical assessment. The Hip & Knee Osteoarthritis Assessment Template can be used to help guide the assessment and to record the details.
1. Asking Five Screening Questions1
1 Arthritis Association of Canada, The College of Family Physicians of Canada, Centre for Effective Practice. Osteoarthritis tool. 2017.
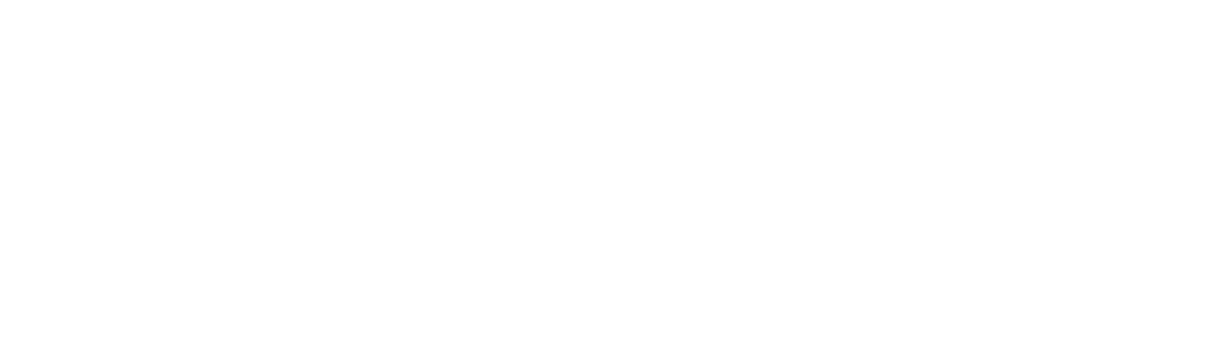
Consider the following screening questions to help rule out other pathologies:
Serious pathologies to screen for:
If inflammatory arthritis or other serious pathologies are identified, then these standards are not the appropriate tool for the individual.
Below is a list of serious pathologies which may require urgent care and/or a different approach to care planning11 Arthritis Association of Canada, The College of Family Physicians of Canada, Centre for Effective Practice. Osteoarthritis tool. 2017.:
Infection
Indication
Fever, meningism, history of immunosuppression or IV drug use
Investigations to consider
x-rays, MRI, CBC
Inflammatory Arthritis
Indication
Rheumatoid arthritis, polymyalgia rheumatica, giant cell arthritis
Investigations to consider
Rhuematology consult and blood tests for ESR, CRP, and rheumatological markers
Fracture
Indication
Osteoporotic fracture, traumatic fall with risk of fracture
Investigations to consider
x-rays, CT
Tumour
Indication
History of cancer, unexplained weight loss, significant night pain, severe fatigue
Investigations to consider
x-rays, MRI
Psychosocial risk factors which may affect diagnosis and care planning
Presence of psychosocial risk factors means the individual will benefit from reassurance and education to reduce chronicity. Reassess psychosocial risk factors for any individual with unimproved or poorly managed pain, after six weeks of treatment.
RISK FACTOR #1: Belief that joint pain is harmful or potentially severely disabling
KEY SCREENING QUESTION: Do you think your pain will improve or become worse?
RISK FACTOR #2:
Fear and avoidance of activity or movement
KEY SCREENING QUESTION: Do you think you would benefit from activity, movement or exercise?
RISK FACTOR #3:
Tendency to low mood and withdrawal from social interaction
KEY SCREENING QUESTION: How are you emotionally coping with your joint pain?
RISK FACTOR #4:
Expectation of passive treatment(s) rather than a belief that active participation will help
KEY SCREENING QUESTION: What treatments or activities do you think will help you recover?
HISTORY
2. Documenting a Thorough Health History
Documenting a thorough health history must include:

- Past medical history of the symptomatic joint
- Joint instability from ligament pathology
- Understanding co-morbidities and their current management

- Identifying the joints with pain or stiffness symptoms
- Mechanical symptoms, possibly from cartilage pathology
- Understanding the individual’s pain experience (intensity, type, when, and sleep quality)

- Understanding the engagement in activities
Consider asking: How many minutes of exercise and/or physical activity (Standard 5) do you do per week? - Screening for falls in the past six months
- Understanding the person’s support network, lifestyle and occupation
Consider asking: “Do you (ever) have difficulties making ends meet?” - Understanding the avoidance of activities because of pain, stiffness or weakness
PHYSICAL EXAM
3. Performing a Physical Exam
The physical examination helps to deepen the understanding of the individual’s disease activity and allows for a baseline collection of information to inform treatment planning over time. It is important to explain the process and ask for consent as the clinician moves through each step of the physical examination.
The examination must include recording the height, weight, body mass index (BMI) and blood pressure. Blood pressure is only necessary for medication modification.
A good examination will include:

- Observation of spinal and general posture
- Observation of knee joint alignment when weight bearing and non-weight bearing
- Scanning of lower extremity to evaluate referred pain and neurological signs
- Observation of joint appearance and presence of swelling in knees only
- Assessment of affected and associated joints’ range of motion, strength and stability tests:
- Internal rotation (hips)
- Flexion (both)
- Use additional investigations to rule out other conditions

- Observation of spinal and general posture
- Observation of knee joint alignment when weight bearing and non-weight bearing
- Assessment of balance
- Observation of gait pattern to test for mobility function
- Timed Up and Go Test66The Arthritis Society. Getting a grip on arthritis: Best practice guidelines. 2017.
- Assessment of risk for falls and/or functional strength of lower extremities using:
- 30-second Sit to Stand Test66The Arthritis Society. Getting a grip on arthritis: Best practice guidelines. 2017.
IMAGING AND REFERRALS
Imaging
Imaging and laboratory investigations are not required to assist with clinical OA diagnosis of typical presentation.33 Bedson J, Croft PR. The discordance between clinical and radiographic knee osteoarthritis: A systematic search and summary of the literature. BMC Musculoskeletal Disorders. 2008;9(1):1-11. doi: https://doi.org/10.1186/1471-2474-9-116.
Clinical diagnosis is sufficient to begin care planning and treatment of OA and clinical presentation, in combination with shared decision-making, should guide the ongoing conservative management of OA. Findings on imaging may not always match the individual’s symptoms, and do not predict the response to treatment.
If the screening questions have indicated further investigation is required or if the diagnosis is uncertain, then the assessing clinician can begin with preliminary imaging (x-rays) and proceed to advanced imaging only if indicated. Preferred x-rays views can be found here.
Repeated use of imaging to track OA progression is not typically warranted. Repeated imaging does not provide added value to treatment planning unless the progression of symptoms is unexpected and an x-ray has not been done in 1-2 years.
Immediate Orthopaedic Surgeon Referral
The goal with these standards is to encourage an adequate trial of non-surgical treatment prior to referral to a surgeon (Standard 8). However, certain criteria warrant urgent referral to an orthopaedic surgeon.
These criteria include:
- Other pathologies are identified:
- Suspected fracture; or
- Ligament injury
- During the documenting of history or the performing of the physical exam the individual with OA describes all of the following:
- Dull/aching pain punctuated by short episodes of unpredictable pain; and
- Pain interrupting sleep; and
- Loss of independence and ability to do self care; and
- Increase of frequency and dosing of pharmacological treatments; and
- Avoidance of all daily activities
- Increased reliance on use of opioids
- Preliminary imaging was appropriately pursued and radiographical evidence reveals a severe joint spacing reduction.
Standard 8 provides more details on a routine referral to surgeon after non-surgical treatment has been exhausted. In Alberta, x-rays are required to refer to an orthopaedic surgeon.
STAGING OSTEOARTHRITIS
Assigning an Osteoarthritis “Stage” to the Individual
Typical terms for OA clinical stages are: ‘early/mild’, ‘moderate’ or ‘advanced/late’. The nine standards will not use ‘clinical stage terms’ to describe an individual’s OA and/or their applicable treatment options.
Clinical presentation should guide the use of these standards and the tailoring of non-surgical treatments is appropriate no matter what the stage of OA (clinical or radiographical) and classification should not discourage or limit individuals from non-surgical treatment options (more in Standard 2 and Standard 3).
Individuals will seek care at different points in their disease journey; a clinician’s diagnosis may be building on care the individual has already received. For instance, an individual may still be ‘early’ but has been managing their condition for some time: their disease activity may be ‘early’ but their journey and their perception of treatment options may be ‘advanced’.
INTRODUCTION
Both regulated and non-regulated clinicians may be involved in the assessment and care of an individual with OA.
Adults (typically aged 40 years and older) who present with joint pain, swelling or stiffness in their hips, knees or lower backs should be assessed thoroughly to determine if they have OA in their knees or hips. 1, 2
1 Arthritis Association of Canada, The College of Family Physicians of Canada, Centre for Effective Practice. Osteoarthritis tool. 2017.
2 The Arthritis Society. Getting a grip on arthritis: Best practice guidelines. 2017.
Osteoarthritis of the hip or knee will likely present with at least one of these symptoms:
- Persistent atraumatic movement-related joint pain
- Aching
- Swelling
- Joint instability due to bone misalignment
- Catching
- Morning stiffness lasting less than 30 minutes
These symptoms may affect more than one joint at a time. Prior injuries, existing comorbidities and congenital deformities may be present along with typical OA symptoms.
If the individual does not have hip and/or knee OA or meets criteria for consideration for inflammatory arthritis then these standards are not appropriate and other guidelines and tools should be used to inform diagnoses and care.
SCREENING
SCREENING
If OA is suspected, a diagnosis can be made with a comprehensive biopsychosocial clinical assessment. The Hip & Knee Osteoarthritis Assessment Template can be used to help guide the assessment and to record the details.
1. Asking Five Screening Questions1
1 Arthritis Association of Canada, The College of Family Physicians of Canada, Centre for Effective Practice. Osteoarthritis tool. 2017.
Consider the following screening questions to help rule out other pathologies:
Serious pathologies to screen for:
If inflammatory arthritis or other serious pathologies are identified, then these standards are not the appropriate tool for the individual.
Below is a list of serious pathologies which may require urgent care and/or a different approach to care planning11 Arthritis Association of Canada, The College of Family Physicians of Canada, Centre for Effective Practice. Osteoarthritis tool. 2017.:
Infection
Indication
Fever, meningism, history of immunosuppression or IV drug use
Investigations to consider
x-rays, MRI, CBC
Inflammatory Arthritis
Indication
Rheumatoid arthritis, polymyalgia rheumatica, giant cell arthritis
Investigations to consider
Rhuematology consult and blood tests for ESR, CRP, and rheumatological markers
Fracture
Indication
Osteoporotic fracture, traumatic fall with risk of fracture
Investigations to consider
x-rays, CT
Tumour
Indication
History of cancer, unexplained weight loss, significant night pain, severe fatigue
Investigations to consider
x-rays, MRI
Psychosocial risk factors which may affect diagnosis and care planning
Presence of psychosocial risk factors means the individual will benefit from reassurance and education to reduce chronicity. Reassess psychosocial risk factors for any individual with unimproved or poorly managed pain, after six weeks of treatment.
RISK FACTOR #1: Belief that joint pain is harmful or potentially severely disabling
KEY SCREENING QUESTION: Do you think your pain will improve or become worse?
RISK FACTOR #2:
Fear and avoidance of activity or movement
KEY SCREENING QUESTION: Do you think you would benefit from activity, movement or exercise?
RISK FACTOR #3:
Tendency to low mood and withdrawal from social interaction
KEY SCREENING QUESTION: How are you emotionally coping with your joint pain?
RISK FACTOR #4:
Expectation of passive treatment(s) rather than a belief that active participation will help
KEY SCREENING QUESTION: What treatments or activities do you think will help you recover?
HISTORY
HISTORY
2. Documenting a Thorough Health History
Documenting a thorough health history must include:

- Past medical history of the symptomatic joint
- Joint instability from ligament pathology
- Understanding co-morbidities and their current management

- Identifying the joints with pain or stiffness symptoms
- Mechanical symptoms, possibly from cartilage pathology
- Understanding the individual’s pain experience (intensity, type, when, and sleep quality)

- Understanding the engagement in activities
Consider asking: How many minutes of exercise and/or physical activity (Standard 5) do you do per week? - Screening for falls in the past six months
- Understanding the person’s support network, lifestyle and occupation
Consider asking: “Do you (ever) have difficulties making ends meet?” - Understanding the avoidance of activities because of pain, stiffness or weakness
PHYSICAL EXAM
PHYSICAL EXAM
3. Performing a Physical Exam
The physical examination helps to deepen the understanding of the individual’s disease activity and allows for a baseline collection of information to inform treatment planning over time. It is important to explain the process and ask for consent as the clinician moves through each step of the physical examination.
The examination must include recording the height, weight, body mass index (BMI) and blood pressure. Blood pressure is only necessary for medication modification.
A good examination will include:

- Observation of spinal and general posture
- Observation of knee joint alignment when weight bearing and non-weight bearing
- Scanning of lower extremity to evaluate referred pain and neurological signs
- Observation of joint appearance and presence of swelling in knees only
- Assessment of affected and associated joints’ range of motion, strength and stability tests:
- Internal rotation (hips)
- Flexion (both)
- Use additional investigations to rule out other conditions

- Observation of spinal and general posture
- Observation of knee joint alignment when weight bearing and non-weight bearing
- Assessment of balance
- Observation of gait pattern to test for mobility function
- Timed Up and Go test66The Arthritis Society. Getting a grip on arthritis: Best practice guidelines. 2017.
- Assessment of risk for falls and/or functional strength of lower extremities using:
- 30-second Sit to Stand test66The Arthritis Society. Getting a grip on arthritis: Best practice guidelines. 2017.
IMAGING AND REFERRALS
IMAGING AND REFERRALS
Imaging
Imaging and laboratory investigations are not required to assist with clinical OA diagnosis of typical presentation.33 Bedson J, Croft PR. The discordance between clinical and radiographic knee osteoarthritis: A systematic search and summary of the literature. BMC Musculoskeletal Disorders. 2008;9(1):1-11. doi: https://doi.org/10.1186/1471-2474-9-116.
Clinical diagnosis is sufficient to begin care planning and treatment of OA and clinical presentation, in combination with shared decision-making, should guide the ongoing conservative management of OA. Findings on imaging may not always match the individual’s symptoms, and do not predict the response to treatment.
Repeated use of imaging to track OA progression is not typically warranted. Repeated imaging does not provide added value to treatment planning unless the progression of symptoms is unexpected and an x-ray has not been done in 1-2 years.
Immediate Orthopaedic Surgeon Referral
The goal with these standards is to encourage an adequate trial of non-surgical treatment prior to referral to a surgeon (Standard 8). However, certain criteria warrant urgent referral to an orthopaedic surgeon.
These criteria include:
- Other pathologies are identified:
- Suspected fracture; or
- Ligament injury
- During the documenting of history or the performing of the physical exam the individual with OA describes all of the following:
- Dull/aching pain punctuated by short episodes of unpredictable pain; and
- Pain interrupting sleep; and
- Loss of independence and ability to do self care; and
- Increase of frequency and dosing of pharmacological treatments; and
- Avoidance of all daily activities.
- Increased reliance on use of narcotics
- Preliminary imaging was appropriately pursued and radiographical evidence reveals a severe joint spacing reduction.
Standard 8 provides more details on a routine referral to surgeon after non-surgical treatment has been exhausted. In Alberta, x-rays are required to refer to an orthopaedic surgeon.
STAGING OSTEOARTHRITIS
STAGING OSTEOARTHRITIS
Assigning an Osteoarthritis “Stage” to the Individual
Typical terms for OA clinical stages are: ‘early/mild’, ‘moderate’ or ‘advanced/late’. The nine standards will not use ‘clinical stage terms’ to describe an individual’s OA and/or their applicable treatment options.
Clinical presentation should guide the use of these standards and the tailoring of non-surgical treatments is appropriate no matter what the stage of OA (clinical or radiographical) and classification should not discourage or limit individuals from non-surgical treatment options (more in Standard 2 and Standard 3).
Individuals will seek care at different points in their disease journey; a clinician’s diagnosis may be building on care the individual has already received. For instance, an individual may still be ‘early’ but has been managing their condition for some time: their disease activity may be ‘early’ but their journey and their perception of treatment options may be ‘advanced’.
Regulated Health Care Professionals
- Family Physicians
- Nurse Practitioners
- Physiotherapists (Allied Health)
- Occupational Therapists (Allied Health)
- Pharmacists (Allied Health)
- Registered Dietitians (Allied Health)
- Psychiatrists
- Psychologists/Mental Health Therapists
- Chiropractors
- Specialty Physicians including:
- Sport and Exercise Medicine Physicians
- Radiologists
- Rheumatologists
- Physiatrists
- Orthopedic Surgeons
Non-regulated Health Care Professionals
- Podiatrists
- Pedorthists
- Kinesiologists
- Exercise Physiologists
- Recreational Therapists
- Counsellors
Differential Diagnosis for OA
The following indications will require additional investigations to identify appropriate diagnosis:
- A recent history of injury
- Joint locking
- Loose body or other joint pathology
- Joint instability
- Prolonged morning joint-related stiffness (greater than 30 minutes)
- Hip or knee pain referred from the lumbar spine
- Hot swollen joints or general ill health
Criteria for consideration of Inflammatory Arthritis
- Pain increased with rest or immobility
- Persistent joint swelling and tenderness
- Frequent joint warmth and/or erythema
- Morning stiffness greater than 30 minutes
- Three or more joints affected
- Unexplained weight loss
Possible related conditions and recommendations for investigation
Shared Decision Making
The inter-twining principles that ground the Comprehensive Quality Care Standards for Osteoarthritis of the Hip and Knee.
Shared decision-making (SDM) techniques and processes are emphasized throughout these standards. The use of SDM is essential to achieving ‘family and patient-centric’ care. SDM is evidence-based and proven to improve outcomes for the individual such as satisfaction with and adherence to care plans.
Standard 2 describes how sharing the decision making is important for building a care plan. This toolkit This toolkit provides more detail on the 3-talk model that can be used to practice SDM in everyday practice.
Preliminary Imaging
- Joint is difficult to examine making the clinical OA diagnosis uncertain
- OA clinical disease activity progresses atypically, and an immediate referral to a surgeon may be appropriate
- Other pathologies are suspected (see below)
- To assist with administering an injection treatments (Standard 7)
- Conservative treatments have been exhausted and a referral to an orthopaedic surgeon is appropriate (Standard 8)
Advanced Imaging
- Other pathologies are suspected (other guidance documents will need to be consulted)
- Ultrasounds are sometimes appropriate to accompany injection treatments (Standard 7)
Preferred Views for Conventional Radiographs
- Anterior-posterior weight bearing
- Lateral
- Skyline*
- Tunnel view*
- Anterior-posterior pelvis centred at pubis
- Anterior-posterior and lateral of proximal half of affected femur
Staging Osteoarthritis
- Various consistent, validated definitions in literature
- Subjective in two dimensions:
- Individual’s perception and reporting.
- Clinician’s perception of individual
- No measurable clinical objectivity
- Validated definitions in radiological literature
- Does not reliably correlate with symptoms22Australian Orthopaedic Association National Joint Replacement Registry. Hip and knee arthroplasty: Annual report 2015. Adelaide, Australia: Australian Orthopaedic Association; 2015.
- Kellgren and Lawrence Radiographic Criteria for Assessment of OA provided in the AAC OA Tool
Clinical presentation should guide the use of these standards and the Conservative OA Treatments Toolbox options is appropriate regardless of OA stage (clinical or radiographical). It would be a disservice to the individual with OA to suggest that a specific ‘OA stage’ limits or discourages treatment options (more in Standard 2 and Standard 3).
The only situation in which radiographical OA classification may alter an approach to care planning is if the person’s OA disease activity triggers the criteria for an immediate referral to an orthopaedic surgeon.
Timed Up and Go Test
Adults (typically aged 40 years and older) who present with joint pain, swelling or stiffness in their hips, knees or lower backs should be considered for an osteoarthritis (OA) assessment. A diagnosis of OA can be made with a comprehensive bio-psychosocial clinical assessment that contains three elements: screening to rule out other possible pathologies, a detailed health history and a physical examination. This form can be used to record findings from each element.
The physical examination helps to deepen the understanding of the individual’s disease activity and allows for a baseline collection of information to inform treatment planning overtime. It is important to explain the process and ask for consent as the clinician moves through each step of the physical examination. Consider the following physical and observational assessments to inform the diagnosis:
- Tests to confirm diagnosis:
- Observation of spinal and general posture
- Observation of knee joint alignment when weight bearing and non-weight bearing
- Scanning of lower extremity to evaluate referred pain and neurological signs
- Observation of joint appearance and presence of swelling in knees only
- Assessment of affected and associated joints’ range of motion, strength and stability tests:
- Internal rotation (hips)
- Flexion (both)
- Collecting a baseline of function:Recording of height, weight, body mass index (BMI) and blood pressure*
- Assessment of balance
- Observation of gait pattern to test for mobility function
- Assessment of risk for falls and/or functional strength of lower extremities using:
*Blood pressure is only necessary for medication modification.
Instructions:
- Instruct the individual
- On the word “go” begin timing
- Stop timing after the individual sits back down
- Record time
Interpretation:
- ≤ 10 seconds = normal
- ≤ 20 seconds = good mobility, can go out alone, mobile without walking support (Standard 7)
- ≤ 30 seconds = concerns, cannot go outside alone, requires walking support (Standard 7)
* A score of ≥ 12 seconds has been shown to indicate a high risk for falls
Age Matched Norms:
| Age | Mean in seconds |
|---|---|
| 20-29 | 8.57 +/- 1.4 |
| 30-39 | 8.56 +/- 1.23 |
| 40-49 | 8.86 +/- 1.88 |
| 50-59 | 9.90 +/- 2.29 |
| 60-69 | 7.9 +/- 0.9 |
| 70-79 | 7.7 +/- 2.3 |
| 80-89 | No device: 11.0 +/- 2.2 With device: 19.9 +/- 6.4 |
| 90-101 | No device: 14.7 +/- 7.9 With device: 19.9 +/- 2.5 |
If any of the following apply, then neurological problems may be present which would require further evaluation:
- Slow tentative pace
- Loss of balance
- Short stride
- Little or no arm swing
- Steadying self on walls
- Shuffling
- En bloc turning
- Not using assistive device properly
Sit to Stand Test
Adults (typically aged 40 years and older) who present with joint pain, swelling or stiffness in their hips, knees or lower backs should be considered for an osteoarthritis (OA) assessment. A diagnosis of OA can be made with a comprehensive bio-psychosocial clinical assessment that contains three elements: screening to rule out other possible pathologies, a detailed health history and a physical examination. This form can be used to record findings from each element.
The physical examination helps to deepen the understanding of the individual’s disease activity and allows for a baseline collection of information to inform treatment planning overtime. It is important to explain the process and ask for consent as the clinician moves through each step of the physical examination. Consider the following physical and observational assessments to inform the diagnosis:
- Tests to confirm diagnosis:
- Observation of spinal and general posture
- Observation of knee joint alignment when weight bearing and non-weight bearing
- Scanning of lower extremity to evaluate referred pain and neurological signs
- Observation of joint appearance and presence of swelling in knees only
- Assessment of affected and associated joints’ range of motion, strength and stability tests:
- Internal rotation (hips)
- Flexion (both)
- Collecting a baseline of function:Recording of height, weight, body mass index (BMI) and blood pressure*
- Assessment of balance
- Observation of gait pattern to test for mobility function
- Assessment of risk for falls and/or functional strength of lower extremities using:
*Blood pressure is only necessary for medication modification.
Instructions:
- Instruct the individual
- On the word “go” begin timing
- Count the number of times the individual comes to a full standing position in 30 seconds
- The count is the individual’s score, compare to below
Interpretation:
A below average score indicates a risk for falls.
| Age | Men | Women |
|---|---|---|
| 60-64 | <14 | <12 |
| 65-69 | <12 | <11 |
| 70-74 | <12 | <10 |
| 75-79 | <11 | <10 |
| 80-84 | <10 | <9 |
| 85-89 | <8 | <8 |
| 90-94 | <7 | <4 |
Alberta Referral Directory
Alberta Referral Directory to assist with:
- Identifying diagnostic imaging locations
- Orthopaedic surgery referral requirements to the Alberta Hip and Knee Program (if appropriate)
- Designing a local Resource Inventory and keeping it up to date
- Referral to other clinicians