STANDARD 8
Individuals with osteoarthritis (OA) of the hip or knee may be considered for joint surgery if they have severe symptoms and poor quality of life that has not improved after exhausting their non-surgical care options. While joint replacements have very positive health outcomes for many individuals and can help them return to conservative treatments faster, non-urgent surgery should be considered an option only after conservative treatments stop working. The use of shared decision-making techniques will ensure individuals understand the benefits and risks of surgical options and help set expectations for functional outcomes.

OVERVIEW
- Referral to a surgeon can be considered if conservative treatments stop working. Surgery is not a goal to achieve, but an advanced pain management option after other conservative treatments have failed
- Joint replacements are very successful procedures for many individuals but there are risks and benefits and the individual has a choice – they are elective procedures
- Use the standardized referral form to refer to one of 11 Albertan Hip and Knee Clinics that all follow the Hip and Knee Surgical Care Path, where the individual will be screened and assessed for candidacy
- Surgical candidacy can be affected by the current medical management of comorbidities, among other criteria
- Successful recovery requires commitment to both supported and self-managed rehabilitation
- Conservative management should continue throughout the wait for surgery and after surgery
INTRODUCTION
Despite optimizing non-surgical options, individuals with osteoarthritis (OA) may still experience a progression of symptoms and deterioration of function and mobility, which impacts their quality of life. At this time, a referral for joint surgery may be appropriate for advanced pain management. An adequate trial of supported conservative care is strongly recommended before joint surgery is considered. This will help to ensure that appropriate candidates are referred for a consult with a surgeon in a timely manner.
This referral decision for joint surgery should be supported with:
- Readiness of the individual and
- Declining trends in patient reported pain, mobility and functional ability (Standard 9)
Individuals who are beyond non-surgical treatment may require an ‘urgent’ referral to surgery.
This standard aligns with the most recent Hip and Knee Surgical Care Path
WHEN TO REFER
If the individual with OA reports a progression of symptoms and functional decline which has not improved after an adequate trial of conservative care (below), a referral for joint surgery may be considered. Indicators of declining conditions include:
- Decreased function and mobility:
- An inability to maintain usual work duties, self-care or daily activities and/or
- An increased reliance on others
- Increased use and dependency on gait aids for activities of daily living:
- Individuals may start with a cane and progress to a walker or wheelchair, to help stabilize themselves and stay mobile
- Increased use and dependency on increasing doses of prescription pain medication or opioids to achieve mobilization
- Pain interrupting sleep and/or
- Documented decline in quantitative patient reported outcome measures (PROMs) (Standard 9)
TRIAL CONSERVATIVE CARE
Education sessions can be delivered in verbal, written and/or virtual formats.
The OA Self Management Education Booklet aligns with the topics for an introduction to OA education and can be provided to the individual with OA as early as first confirmation of diagnosis. There is also an accompanying Powerpoint presentation for the booklet. Examples of publicly available materials are provided in the Health Resources Matrix.
Look for community organizations as well as health organizations to find applicable educational programs. For instance, a recreation centre may have an OA focused class. Build relationships with local educational programs and keep a Resource Inventory up to date with the program schedule for these classes and to ensure individuals with OA are directed to the program that is most applicable to their gaps in knowledge.
If there are no local education programs running in the area, consider running one. Consider using group teaching to build a community for individuals with OA to connect with one another. Locally developed materials should align with these standards, the Conservative OA Treatments and best evidence. Successful education material should be presented in ‘patient friendly’ language and offer opportunities for interaction and question answering. Consider partnering with other agencies or programs as well to deliver a multi-disciplinary approach.
STARTING & COMPLETING REFERRAL
Before referring an individual for surgical consultation, the Primary Clinician should advise the individual that there are risks and benefits of surgical joint replacement, and there should be a discussion about appropriate expectations for functional outcome after surgery. Surgical options for hip or knee OA can include total joint replacements, partial replacements (hemiarthroplasty), joint resurfacing, and revisions. It is important to discuss whether surgery would effectively meet the individual’s health needs and evaluate their willingness to undergo the surgical preparation and rehabilitation processes. Although, the surgeon will explain the details of any risk factors with the individual, the referring clinician should discuss with the individual that:
- They may or may not be a suitable candidate for surgery as per the Hip and Knee Surgical Care Path
- Certain factors like the presence of comorbidities will have to be adequately optimized prior to approval for surgery.
Once the individual provides informed consent for the coordination of a referral, they may be guided through the process. Refer to the provincially standardized Hip and Knee Referral Form and the Alberta Referral Directory to refer the individual to one of the eleven Albertan hip and knee central intake clinics.
The referral form should be complete and compiled with the required appropriate x-rays, additional applicable details on medical history and a history of the conservative treatments trialed to date. If the referral is not complete, the referring clinic will send the original referral form back to the referring clinician and request outstanding information. This should be avoided as it may result in delays for the individual’s wait times for surgeon consult.
Support the individual with OA to understand that their first assessment at the Hip and Knee Central Intake Clinic will be screened to evaluate whether they are an appropriate candidate for surgery, and a consult with a surgeon may follow after that. Candidacy for surgery will be evaluated at the surgeon consult again. It is important to empower the individual with OA to take an active role in discussing the criteria for surgery and the status of their comorbidities with both the specialist screening physician (if applicable) and the surgeon. It is also important to emphasize that their OA care will not end if surgery is not the correct step for them (see below).
An individual’s candidacy for surgery may evolve with time. Collaboration between the individual and all clinicians (including the screening specialist and/or surgeon) is essential to ensure up to date information about symptoms and quality of life is documented and the individual’s care plan is current.
With the full implementation of these standards the relationship between referring clinician and surgeon will shift over time. A more equal partnership in optimizing the individual with OA for surgery will be possible with a broader understanding of conservative OA management and the criteria for risk reduction prior to surgery.
Steroid injections should not be performed less than six weeks before the date of surgery.
SURGICAL CARE PATH
The Hip and Knee Surgical Care Path is authored by the Albertan Hip and Knee Replacement Clinical Committee. The Clinical Committee is a partnership between the Alberta Orthopaedic Society and the Bone and Joint Health Strategic Clinical Network.
As well as inpatient care requirements for hip or knee joint replacement, the care path details criteria for:
- Referral to an Albertan Hip and Knee Clinic;
- The contact information for the clinics can be located on the Alberta Referral Directory (see the Health Resource Matrix for more information);
- Surgical candidacy.
It is recognized that clinician familiarity with the Hip and Knee Surgical Care Path is limited outside of the orthopaedic surgeons’ practices. With the full implementation of these standards, the familiarity with the care path will grow over time.
Referral to orthopaedic surgeons at their central-intake hip and knee clinics does vary in Alberta, despite the Hip and Knee Surgical Care Path. This is because surgeons’ practices vary slightly across the province: some surgeons offer individuals a variety of non-surgical OA treatment options, other surgeons do not include OA management treatments in their scope of work. With the implementation of this standard, the OA treatment trial period will be formalized, regardless of the clinician supporting that trial.
SURGICAL CANDIDACY
Pain medications must be prescribed very carefully, and a full history of the individual’s active prescriptions, history of addictions, comorbidities and pain experience must be evaluated. Based on the pharmaceutical treatment algorithm, develop a tailored medication plan taking into consideration the individual’s symptoms, ability to participate in Core Treatments, other health conditions, values and preferences.
Use the Resource Inventory to track which Adjunct Treatments are available locally. Use the Tables of Examples of Conservative OA Treatments to consider the breadth of options for adjunct treatments.
Standard 3 describes how it is every clinician’s responsibility to communicate to the Primary Clinician, and vice versa. Any changes in the care plan or health status of the individual should be communicated. This is particularly important for the management of pharmacological treatments. Communications between clinicians can emphasize that the goal is to provide Adjunct Treatments to encourage return to Core Treatments.
At all follow-up visits, work with your individual with OA to reassess, track, and modify their Adjunct Treatments to better reflect their current needs and progress. This collaborative process will improve commitment to Core Treatments.
ONGOING MANAGEMENT
It is important to note that conservative (non-surgical) care does not stop after:
- A referral for joint surgery
- The decision and wait-listing for surgery nor
- The surgery
The continuation of conservative treatments will:
- Help individuals optimize their general health pre-operatively
- Improve their chances for greater functional recovery after surgery and
- Improve their general health and joint care long after the surgery
- Joint care includes the care of replaced joints as well as the care of joints still at risk of requiring replacement.
At follow-up visits, after surgery, continue to recommend appropriate conservative management options in order to conserve the repaired joint, speed recovery, maximize function and conserve other joints.
INTRODUCTION
Despite optimizing non-surgical options, individuals with osteoarthritis (OA) may still experience a progression of symptoms and deterioration of function and mobility, which impacts their quality of life. At this time, a referral for joint surgery may be appropriate for advanced pain management. An adequate trial of supported conservative care is strongly recommended before joint surgery is considered. This will help to ensure that appropriate candidates are referred for a consult with a surgeon in a timely manner.
This referral decision for joint surgery should be supported with:
- Readiness of the individual and
- Declining trends in patient reported pain, mobility and functional ability (Standard 9)
Individuals who are beyond non-surgical treatment may require an ‘urgent’ referral to surgery.
This standard aligns with the most recent Hip and Knee Surgical Care Path
WHEN TO REFER
- Decreased function and mobility:
- An inability to maintain usual work duties, self-care or daily activities and/or
- An increased reliance on others
- Increased use and dependency on gait aids for activities of daily living:
- Individuals may start with a cane and progress to a walker or wheelchair, to help stabilize themselves and stay mobile
- Increased use and dependency on increasing doses of prescription pain medication or opioids to achieve mobilization
- Pain interrupting sleep and/or
- Documented decline in quantitative patient reported outcome measures (PROMs) (Standard 9)
TRIAL CONSERVATIVE CARE
The OA Self Management Education Booklet aligns with the topics for an introduction to OA education and can be provided to the individual with OA as early as first confirmation of diagnosis. There is also an accompanying Powerpoint presentation for the booklet. Examples of publicly available materials are provided in the Health Resources Matrix.
Look for community organizations as well as health organizations to find applicable educational programs. For instance, a recreation centre may have an OA focused class. Build relationships with local educational programs and keep a Resource Inventory up to date with the program schedule for these classes and to ensure individuals with OA are directed to the program that is most applicable to their gaps in knowledge.
If there are no local education programs running in the area, consider running one. Consider using group teaching to build a community for individuals with OA to connect with one another. Locally developed materials should align with these standards, the Conservative OA Treatments and best evidence. Successful education material should be presented in ‘patient friendly’ language and offer opportunities for interaction and question answering. Consider partnering with other agencies or programs as well to deliver a multi-disciplinary approach.
STARTING & COMPLETING REFERRAL
- They may or may not be a suitable candidate for surgery as per the Hip and Knee Surgical Care Path
- Certain factors like the presence of comorbidities will have to be adequately optimized prior to approval for surgery.
Once the individual provides informed consent for the coordination of a referral, they may be guided through the process. Refer to the provincially standardized Hip and Knee Referral Form and the Alberta Referral Directory to refer the individual to one of the eleven Albertan hip and knee central intake clinics.
The referral form should be complete and compiled with the required appropriate x-rays, additional applicable details on medical history and a history of the conservative treatments trialed to date. If the referral is not complete, the referring clinic will send the original referral form back to the referring clinician and request outstanding information. This should be avoided as it may result in delays for the individual’s wait times for surgeon consult.
Support the individual with OA to understand that their first assessment at the Hip and Knee Central Intake Clinic will be screened to evaluate whether they are an appropriate candidate for surgery, and a consult with a surgeon may follow after that. Candidacy for surgery will be evaluated at the surgeon consult again. It is important to empower the individual with OA to take an active role in discussing the criteria for surgery and the status of their comorbidities with both the specialist screening physician (if applicable) and the surgeon. It is also important to emphasize that their OA care will not end if surgery is not the correct step for them (see below).
An individual’s candidacy for surgery may evolve with time. Collaboration between the individual and all clinicians (including the screening specialist and/or surgeon) is essential to ensure up to date information about symptoms and quality of life is documented and the individual’s care plan is current.
With the full implementation of these standards the relationship between referring clinician and surgeon will shift over time. A more equal partnership in optimizing the individual with OA for surgery will be possible with a broader understanding of conservative OA management and the criteria for risk reduction prior to surgery.
Steroid injections should not be performed less than six weeks before the date of surgery.
SURGICAL CARE PATH
As well as inpatient care requirements for hip or knee joint replacement, the care path details criteria for:
- Referral to an Albertan Hip and Knee Clinic;
- The contact information for the clinics can be located on the Alberta Referral Directory (see the Health Resource Matrix for more information);
- Surgical candidacy.
It is recognized that clinician familiarity with the Hip and Knee Surgical Care Path is limited outside of the orthopaedic surgeons’ practices. With the full implementation of these standards, the familiarity with the care path will grow over time.
Referral to orthopaedic surgeons at their central-intake hip and knee clinics does vary in Alberta, despite the Hip and Knee Surgical Care Path. This is because surgeons’ practices vary slightly across the province: some surgeons offer individuals a variety of non-surgical OA treatment options, other surgeons do not include OA management treatments in their scope of work. With the implementation of this standard, the OA treatment trial period will be formalized, regardless of the clinician supporting that trial.
SURGICAL CANDIDACY
Pain medications must be prescribed very carefully, and a full history of the individual’s active prescriptions, history of addictions, comorbidities and pain experience must be evaluated. Based on the pharmaceutical treatment algorithm, develop a tailored medication plan taking into consideration the individual’s symptoms, ability to participate in Core Treatments, other health conditions, values and preferences.
Use the Resource Inventory to track which Adjunct Treatments are available locally. Use the Tables of Examples of Conservative OA Treatments to consider the breadth of options for adjunct treatments.
Standard 3 describes how it is every clinician’s responsibility to communicate to the Primary Clinician, and vice versa. Any changes in the care plan or health status of the individual should be communicated. This is particularly important for the management of pharmacological treatments. Communications between clinicians can emphasize that the goal is to provide Adjunct Treatments to encourage return to Core Treatments.
At all follow-up visits, work with your individual with OA to reassess, track, and modify their Adjunct Treatments to better reflect their current needs and progress. This collaborative process will improve commitment to Core Treatments.
ONGOING MANAGEMENT
- A referral for joint surgery
- The decision and wait-listing for surgery nor
- The surgery
The continuation of conservative treatments will:
- Help individuals optimize their general health pre-operatively
- Improve their chances for greater functional recovery after surgery and
- Improve their general health and joint care long after the surgery
- Joint care includes the care of replaced joints as well as the care of joints still at risk of requiring replacement.
At follow-up visits, after surgery, continue to recommend appropriate conservative management options in order to conserve the repaired joint, speed recovery, maximize function and conserve other joints.
Immediate or ‘Urgent’ Referral to Orthopaedic Surgeon
The goal with these standards is to encourage an adequate trial of non-surgical (conservative) OA treatment prior to referral to a surgeon (Standard 8). However, there are certain criteria that would result in an ‘urgent’ classification of the individual, and therefore warrant immediate referral to an orthopaedic surgeon. The individual’s experience is very important to consider as an arthroplasty has positive health outcomes for many individuals and can help them return to OA management faster.
Refer immediately to an orthopaedic surgeon if:
- Other pathologies are identified:
- Suspected fracture or
- Ligament injury
- During the documenting of history or the performing of the physical exam the individual with OA describes all of the following:
- Dull/aching pain punctuated by short episodes of unpredictable pain; and
- Pain interrupting sleep; and
- Loss of independence and ability to do self care; and
- Increase of frequency and dosing of pharmacological treatments; and
- Avoidance of all daily activities.
- Increased reliance on use of opioids
- Preliminary imaging was appropriately pursued and radiographical evidence reveals a severe joint spacing reduction.
Hip and Knee Surgical Care Path
The Hip and Knee Surgical Care Path is authored by the Alberta Hip and Knee Replacement Clinical Committee. The Clinical Committee is a partnership between the Alberta Orthopaedic Society and the Bone and Joint Health Strategic Clinical Network.
As well as inpatient care requirements for hip or knee joint replacement, the care path details criteria for:
- Referral to an Albertan Hip and Knee Clinic
- The contact information for the clinics can be located on the Alberta Referral Directory (see the Health Resource Matrix for more information)
- Surgical candidacy
It is recognized that clinician familiarity with the Hip and Knee Surgical Care Path is limited outside of the orthopaedic surgeons’ practices. With the full implementation of these standards, the familiarity with the care path will grow over time.
Referral to orthopaedic surgeons at their central-intake hip and knee clinics does vary in Alberta, despite the Hip and Knee Surgical Care Path. This is because surgeons’ practices vary slightly across the province: some surgeons offer individuals a variety of non-surgical OA treatment options, other surgeons do not include OA management treatments in their scope of work. With the implementation of this standard, the OA treatment trial period will be formalized, regardless of the clinician supporting that trial.
Surgical Candidacy
An individual with osteoarthritis (OA) is not an appropriate candidate for elective hip or knee joint replacement surgery in Alberta if:
- Cognitive/neurologic impairment is present.
- Orthopaedic challenges are present, such as
- A history of infection in the joint
- The surgery is technically unfeasible or
- The joint cannot be reconstructed.
- The individual is not willing or able to be compliant with the care path, which includes:
- Being willing to undergo the surgical optimization and health management protocols prescribed by the surgeon.
- This includes attending the Hip and Knee Surgical Care Path prescribed pre-operative teaching class and [Note that the ‘pre-operative teaching class’ is not equivalent but complementary to non-surgical OA education, for the appropriate audience of confirmed surgical candidates.]
- Being willing to commit to the rehabilitation after the surgery.
- Being willing to undergo the surgical optimization and health management protocols prescribed by the surgeon.
- An extreme medical risk is present (see below).
- There is no demonstrated decline in patient reported outcome measures (PROMs) (Standard 9).
- At least 12 weeks of OA management treatments have not been trialled and documented.
Note: capture of formal PROMs varies across the province and may represent some administrative obstacles to a clinic/clinician. With the full implementation of these standards these obstacles will be overcome with time through the support of the Bone and Joint Health Strategic Clinical Network (BJH SCN) and its collaborators (Standard 9).
Often surgeons will not recommend elective (non emergent) joint replacement surgery for individuals with unmanaged comorbidities that carry excessive medical risk for the surgery, such as:
- Cerebral vascular diseases
- Diabetes
- Cancer
- Heart disease
- Renal disease
- Hepatic disease
- Obesity
If the individual is managing their comorbidities, evaluation of candidacy will be a discussion with the surgeon. If comorbidities are unmanaged, pre-operative surgical optimization at the Hip and Knee Central Intake Clinic may be appropriate, or the individual may need to return to their Primary Clinician to create care plans for their other conditions. The Hip and Knee Central Intake Clinic is responsible for communicating their decision about surgical candidacy and any medical recommendations back to the primary referring clinician, typically by letter.
Note: surgeons’ practices vary slightly across the province: some surgeons offer individuals a variety of non-surgical OA treatment options, other surgeons do not include OA management treatments in their scope of work. With the implementation of this standard, the OA treatment trial period will be formalized, regardless of the clinician supporting that trial.
Additional Investigation Information
Imaging and laboratory investigations are not required to assist with clinical OA diagnosis of typical presentation. A clinical diagnosis is sufficient to begin care planning and treatment of OA and clinical presentation, in combination with shared decision-making, should guide the ongoing management of OA. Imaging findings may not always match the individual’s symptoms, and do not predict the response to treatment.
If the screening questions have indicated further investigation is required or if the diagnosis is uncertain, then consider imaging. The assessing clinician can begin with preliminary imaging and proceed to advanced imaging only if indicated.
| Category | Preliminary Imaging | Advanced Imaging – to be avoided for Hip and Knee OA |
|---|---|---|
| Types of Imaging | X-rays, weight bearing if possible (details below) |
|
| Appropriate Use |
|
|
If Imaging Indicated, Preferred X-ray Views for Hip or Knee OA
If preliminary imaging is indicated, then the follow x-ray views are appropriate for hip and knee OA and all should be captured when weight bearing, if the individual with OA can manage this. Most views in the table are also those requested by orthopaedic surgeons for the provincially standardized hip and knee arthroplasty referral.
| Knee | Hip |
|---|---|
|
|
Notes:
- Skyline x-ray is optional for arthroplasty referral.
- Tunnel view x-ray: is an anterior-posterior weight bearing at 30° flexion of the knee. This view is optional for arthroplasty referral.
Note: repeated use of x-rays to track OA progression is not typically warranted. Repeated x-rays do not provide added value to treatment planning unless the progression of symptoms is unexpected and an x-ray has not been done in 1-2 years.
An Adequate Trial of Conservative Care
It is important to acknowledge that individuals seek system-supported care for their OA at different points in their OA progression. Some individuals seek support early in their OA disease activity and will have many conservative treatment options available to them. Other individuals seek support at a later point of progression and quality of life of the individual may have already declined. Therefore, conservative care should be trialed for at least 12 weeks. Twelve weeks is:
- The reasonable period for an individual to see changes from commitment to exercise, physical activity and/or weight management, and determine if conservative treatments will be appropriate to the individual; and
- A reasonable period to try options, that the individual may not have had or known about before.
It is important to recognize that the 12 weeks trial of conservative care is supportive of (and not opposing to) the success with surgical outcomes
Shared Decision Making
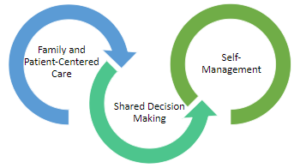
The inter-twining principles that ground the Comprehensive Quality Care Standards for Osteoarthritis of the Hip and Knee.
Shared decision-making (SDM) techniques and processes are emphasized throughout these standards. The use of SDM is essential to achieving ‘family and patient-centric’ care. SDM is evidence-based and proven to improve outcomes for the individual such as satisfaction with and adherence to care plans.
Standard 2 describes how sharing the decision making is important for building a care plan. This toolkit This toolkit provides more detail on the 3-talk model that can be used to practice SDM in everyday practice.
Introductory Education Class on Osteoarthritis
An introduction to Osteoarthritis (OA) class should include the following topics:
- Overview of OA: Causes, symptoms and prognosis
- Self-management strategies:
- Daily symptom management through:
- Application of thermotherapies; and
- Activity self-selection.
- Healthy behaviours and lifestyle modifications:
- Nutrition; and
- Physical activity.
- Daily symptom management through:
- Core Treatments and Adjunct Treatments and the strength of evidence available for each
- Importance of each Core Treatment: education, exercise and physical activity, and weight management
- Safe movements for joints;
- Benefits and risks of Pharmacological and Non-Pharmacological treatments;
- Safe use of walking aids and assistive devices;
- The role of the Primary Clinician and how supporting clinicians will have different expertise to support other treatments;
- The importance of making a care plan with specific goals and updating that care plan as symptoms and life evolve; and
- Tracking symptoms and treatment trials.
BONE & JOINT HEALTH STRATEGIC CLINICAL NETWORK (SCN)
Strategic Clinical Networks (SCNs) are mandated to create improvements within focused areas of health care. They are networks of people who are passionate and knowledgeable about specific areas of health. They are tasked with finding new and innovative ways of delivering care that will provide better quality, better outcomes and better value for every Albertan.
BJH SCN Vision: Keeping Albertans Moving.
BJH SCN Mission: To create a person-centred, integrated system to optimize bone and joint health of Albertans by working together with our partners.
Website: BJH SCN Website
Transformational Road Map: BJH SCN’s Transformational Road Map for 2020-2025