STANDARD 6

OVERVIEW
Key Messages for Weight Management
Carrying extra body weight:
- Exerts additional mechanical stress on the lower limb joints; and
- May have a metabolic link to the disease progression
Over time, increased stress on the joints from extra body weight can result in the production of inflammatory mediators from fat tissue, negatively impacting the health of joint cartilage, and causing loss of muscle mass and strength. Effective weight management explores a wide range of strategies based on the individual’s needs and goals.
Healthy and safe weight management should be considered for all individuals with OA, but reducing extra body weight may be one goal of those individuals who have obesity. Obesity is a chronic medical condition characterized by an excessive accumulation of body fat; it is a significant comorbidity in individuals with OA. Effective weight management explores a wide range of strategies based on the individual’s needs and goals. Use shared decision-making techniques to build a plan that considers:
- Nutritional and/or weight management services to support lifestyle intervention and behaviour modification
- Coordination with exercise and physical activity plans
- Mental health support
- Referral to appropriate supporting clinicians to assist with:
- Pharmacological treatments or Surgery
KEY RESOURCES
- Obesity Primary Health Care Resource Centre
- Helping Adults with Obesity Who Have Functional Concerns
- Nutrition Guidelines, specifically the “Adult Obesity Care” Guideline
- Diabetes, Obesity and Nutrition SCN
- Consider using these modules and resources to support your clinic in becoming more Bariatric Friendly
As well as this: Checklist for Creating Inclusivity - Weight Management Workshops for Clinicians
- Referral to Bariatric Specialty Clinics – Search on Alberta Referral Directory
- Obesity Canada, specifically the Clinical Practice Guidelines and the Reducing Weight Bias Statement
- Bone and Joint Health SCN White Paper on Obesity and OA
- Edmonton Obesity Staging System
- Waist Circumference Measurement Guidelines
- Shared Decision-Making Toolkit
- OA Self Management Toolkit
- SAMPLE Resource Inventory
- TEMPLATE Resource Inventory
- FORM to Document/Modify a Care Plan for Management of OA
- Tables of Examples for the Treatment Toolbox
- Health Change Methodology
INTRODUCTION
A higher body weight and excess body fat have been linked with the development and progression of osteoarthritis (OA). This is due to additional mechanical stresses on the lower limb joints with higher body weight, and a metabolic and inflammatory relationship between body fat and OA disease progression11Godziuk K, Kania-Richmond A, Hart D. Obesity: Implications for patients with osteoarthritis.. Therefore, weight maintenance, or prevention of weight gain, is a foundational strategy in OA management. This is particularly important due to the risks of weight gain associated with both aging and inactivity.
Weight reduction may also be beneficial for reducing OA symptoms and slowing disease progression.
Studies have shown that losing 5-10% of body weight can reduce joint forces/stresses and improve OA-related pain, physical function, and quality of life. Behaviour-based weight management approaches (using nutrition, activity and behavioural control strategies) usually result in sustained weight loss of 3-5% of body weight, however this could still be effective to improve symptoms.
For individuals who are overweight or obese, weight reduction may also be beneficial for reducing OA symptoms and slowing disease progression.
Although sustained weight loss might support reduction of symptoms, the body has mechanisms to defend against weight loss, and most individuals experience weight gain. Therefore, strategies and recommendations around weight management should focus on improvements in overall health, OA symptoms, and physical function rather than weight lost or numbers on a scale. Changing body composition (decreasing body fat without weight change) may also be beneficial.
Body Mass Index (BMI) is a screening tool used to classify normal, overweight and obesity in adults. It is calculated by dividing weight in kilograms by height in metres squared (kg/m2). BMI only provides information about body size. It is not useful to identify the health status of an individual. When used in combination with waist circumference, it can indicate risk for obesity related illness such as diabetes, hypertension and cardiovascular disease. Another tool is the Edmonton Obesity Staging System33Sharma AM, Kushner RF. A proposed clinical staging system for obesity. International Journal of Obesity. 2009;33(3):289-95. (EOSS). The EOSS is a classification system which takes into account the comorbidRueda-Clausen CF, Poddar M, Lear SA, Poirier P, Sharma AM. Canadian Adult Obesity Clinical Practice Guidelines: Assessment of People Living with Obesity. and functional impact obesity has on an individual’s health to determine their stage of obesity (stage 0-4) and guide treatment options.33Sharma AM, Kushner RF. A proposed clinical staging system for obesity. International Journal of Obesity. 2009;33(3):289-95.
COLLABORATING ON WEIGHT MANAGEMENT
Weight bias is the negative attitudes, beliefs and assumptions towards individuals with obesity. One of the most important strategies to reduce weight bias is self-awareness. Clinicians should identify and address their own personal assumptions and attitudes about weight. Several resources are available including the Canadian Adult Obesity Clinical Practice Guidelines: Reducing Weight bias in Obesity Management Practice and Policy.
Understanding the individual’s health priorities, goals, values and preferences is the starting point for having a discussion around weight management for OA. This includes asking the individual for permission to discuss body weight, assessing their weight history, previous and current behaviour management strategies, and interest in additional strategies or supports. Caution and supervision around weight management may be needed in individuals who are at-risk for conditions such as malnutrition or sarcopenia.
Malnutrition and sarcopenic obesity would significantly complicate the person’s efforts to participate in their OA treatment, and therefore these treatments should be addressed first.66Godziuk K, Prado CM, Woodhouse LJ, Forhan M. The impact of sarcopenic obesity on knee and hip osteoarthritis: A scoping review. BMC Musculoskeletal Disorders. 2018;19(1):1-10.
All people, regardless of body size, are equally as susceptible to malnutrition and sarcopenia4, 54Lee S, Kim TN, Kim SH. Sarcopenic obesity is more closely associated with knee osteoarthritis than is nonsarcopenic obesity: A cross‐sectional study. Arthritis & Rheumatism. 2012;64(12):3947-54.
5Jin WS, Choi EJ, Lee SY, Bae EJ, Lee T-H, Park J. Relationships among obesity, sarcopenia, and osteoarthritis in the elderly. Journal of Obesity & Metabolic Syndrome. 2017;26(1):36–44..
There are a range of strategies available to support weight management in OA based on the individual’s needs. Use shared decision-making techniques to create a plan that is tailored to the individual’s goals, values and preferences. This may incorporate:7, 87Kahan S. Overweight and obesity management strategies. The American Journal of Managed Care. 2016;22(7):S186-S96.
8Obesity Canada. Canadian Adult Obesity Clinical Practice Guidelines (CPGs) Edmonton, Alberta: Obesity Canada; 2020 [Available from: https://obesitycanada.ca/guidelines/chapters/. :
- Weight management services to support lifestyle intervention and behaviour interventions (nutrition, physical activity, sleep, stress reduction), to help the individual reach their health goal.
- Examples provided in the Health Resource Matrix, in the Treatment Menu and on the Tables of Examples for the OA Treatments Toolbox.
- Coordination and complementation with the individual’s exercise and physical activity care plan (Standard 5).
- Referral to supports for mental health or psychotherapy, which may assist with managing sleep, stress, and chronic pain as well as eating behaviours such as emotional eating.
- Referral to appropriate supporting clinicians
- Possibly including referral to specialized multidisciplinary care for individuals with obesity.
CONTINUING EDUCATION
For some clinicians the skills required for offering the support described in this standard may be an evolving skill set. There are a number of resources provided in the Health Resources Matrix to explore continuing education.
INTRODUCTION
A higher body weight and excess body fat have been linked with the development and progression of osteoarthritis (OA). This is due to additional mechanical stresses on the lower limb joints with higher body weight, and a metabolic and inflammatory relationship between body fat and OA disease progression11Godziuk K, Kania-Richmond A, Hart D. Obesity: Implications for patients with osteoarthritis.. Therefore, weight maintenance, or prevention of weight gain, is a foundational strategy in OA management. This is particularly important due to the risks of weight gain associated with both aging and inactivity.
Weight reduction may also be beneficial for reducing OA symptoms and slowing disease progression.
Studies have shown that losing 5-10% of body weight can reduce joint forces/stresses and improve OA-related pain, physical function, and quality of life. Behaviour-based weight management approaches (using nutrition, activity and behavioural control strategies) usually result in sustained weight loss of 3-5% of body weight, however this could still be effective to improve symptoms.
For individuals who are overweight or obese, weight reduction may also be beneficial for reducing OA symptoms and slowing disease progression.
Although sustained weight loss might support reduction of symptoms, the body has mechanisms to defend against weight loss, and most individuals experience weight gain. Therefore, strategies and recommendations around weight management should focus on improvements in overall health, OA symptoms, and physical function rather than weight lost or numbers on a scale. Changing body composition (decreasing body fat without weight change) may also be beneficial.
Body Mass Index (BMI) is a screening tool used to classify normal, overweight and obesity in adults. It is calculated by dividing weight in kilograms by height in metres squared (kg/m2). BMI only provides information about body size. It is not useful to identify the health status of an individual. When used in combination with waist circumference, it can indicate risk for obesity related illness such as diabetes, hypertension and cardiovascular disease. Another tool is the Edmonton Obesity Staging System33Sharma AM, Kushner RF. A proposed clinical staging system for obesity. International Journal of Obesity. 2009;33(3):289-95. (EOSS). The EOSS is a classification system which takes into account the comorbidRueda-Clausen CF, Poddar M, Lear SA, Poirier P, Sharma AM. Canadian Adult Obesity Clinical Practice Guidelines: Assessment of People Living with Obesity. and functional impact obesity has on an individual’s health to determine their stage of obesity (stage 0-4) and guide treatment options.33Sharma AM, Kushner RF. A proposed clinical staging system for obesity. International Journal of Obesity. 2009;33(3):289-95.
COLLABORATING ON WEIGHT MANAGEMENT
Understanding the individual’s health priorities, goals, values and preferences is the starting point for having a discussion around weight management for OA. This includes asking the individual for permission to discuss body weight, assessing their weight history, previous and current behaviour management strategies, and interest in additional strategies or supports. Caution and supervision around weight management may be needed in individuals who are at-risk for conditions such as malnutrition or sarcopenia.
Malnutrition and sarcopenic obesity would significantly complicate the person’s efforts to participate in their OA treatment, and therefore these treatments should be addressed first.66Godziuk K, Prado CM, Woodhouse LJ, Forhan M. The impact of sarcopenic obesity on knee and hip osteoarthritis: A scoping review. BMC Musculoskeletal Disorders. 2018;19(1):1-10.
All people, regardless of body size, are equally as susceptible to malnutrition and sarcopenia4, 54Lee S, Kim TN, Kim SH. Sarcopenic obesity is more closely associated with knee osteoarthritis than is nonsarcopenic obesity: A cross‐sectional study. Arthritis & Rheumatism. 2012;64(12):3947-54.
5Jin WS, Choi EJ, Lee SY, Bae EJ, Lee T-H, Park J. Relationships among obesity, sarcopenia, and osteoarthritis in the elderly. Journal of Obesity & Metabolic Syndrome. 2017;26(1):36–44..
There are a range of strategies available to support weight management in OA based on the individual’s needs. Use shared decision-making techniques to create a plan that is tailored to the individual’s goals, values and preferences. This may incorporate:7, 87Kahan S. Overweight and obesity management strategies. The American Journal of Managed Care. 2016;22(7):S186-S96.
8Obesity Canada. Canadian Adult Obesity Clinical Practice Guidelines (CPGs) Edmonton, Alberta: Obesity Canada; 2020 [Available from: https://obesitycanada.ca/guidelines/chapters/. :
- Weight management services to support lifestyle intervention and behaviour interventions (nutrition, physical activity, sleep, stress reduction), to help the individual reach their health goal.
- Examples provided in the Health Resource Matrix, in the Treatment Menu and on the Tables of Examples for the OA Treatments Toolbox.
- Coordination and complementation with the individual’s exercise and physical activity care plan (Standard 5).
- Referral to supports for mental health or psychotherapy, which may assist with managing sleep, stress, and chronic pain as well as eating behaviours such as emotional eating.
- Referral to appropriate supporting clinicians
- Possibly including referral to specialized multidisciplinary care for individuals with obesity.
CONTINUING EDUCATION
For some clinicians the skills required for offering the support described in this standard may be an evolving skill set. There are a number of resources provided in the Health Resources Matrix to explore continuing education.
Shared Decision Making
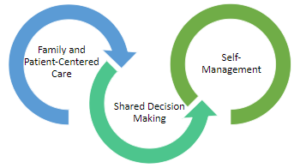
The inter-twining principles that ground the Comprehensive Quality Care Standards for Osteoarthritis of the Hip and Knee.
Shared decision-making (SDM) techniques and processes are emphasized throughout these standards. The use of SDM is essential to achieving ‘family and patient-centric’ care. SDM is evidence-based and proven to improve outcomes for the individual such as satisfaction with and adherence to care plans.
Standard 2 describes how sharing the decision making is important for building a care plan. This toolkit This toolkit provides more detail on the 3-talk model that can be used to practice SDM in everyday practice.
Alberta Referral Directory
Alberta Referral Directory to assist with:
- Identifying diagnostic imaging locations
- Orthopaedic surgery referral requirements to the Alberta Hip and Knee Program (if appropriate)
- Designing a local Resource Inventory and keeping it up to date
- Referral to other clinicians
Resource Inventory Notes
Resource Inventory Notes:
- Form clinic partnerships to create a common Resource Inventory for your local region
- Assign one person to review and update the Resource Inventory regularly
- Build relationships with the services listed on your Resource Inventory to make transition between care as smooth as possible for the individual with OA
- Keep accurate records of cost and wait times for local services to assist individuals wherever possible
OA Self Management Toolkit
OA Self Management Toolkit, Includes:
OA Self Management Toolkit, Includes:
Referral Between Clinicians
The following matrix is provided to guide clinicians on referrals and building a multi-disciplinary team of support for an individual with osteoarthritis (OA). Some supporting clinicians will work in a dedicated team at the same centre as a Primary Clinician, other supporting clinicians will work at separate organizations in the community.
| Category of OA Treatments | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Discipline that may offer the treatment | Education | Exercise and Physical Activity | Weight Management | Supports (Walking and Environmental | Cognitive Behavioural Therapy | Inter-disciplinary Self-Management Programs | Non-prescription Pharma Treatments | Prescription Pharma Treatments | Intra-articular Injections |
| Family Physicians | X | X* | X | X | X* | ||||
| Nurses | X | X | X | X* | |||||
| Physiotherapists | X | X | X | X* | X | Restricted | |||
| Occupational Therapists | X | X | X | X* | X | ||||
| Kinesiologists | X | X | X | ||||||
| Exercise Physiologists | X | X | X | ||||||
| Sport and Exercise Medicine Physicians | X | X | X | X | X | ||||
| Radiologists | X | ||||||||
| Rheumatologists | X | X | X | X | |||||
| Physiatrists | X | X | X | X | |||||
| Chiropractors | X | ||||||||
| Orthopaedic Surgeons | X | X | X | X | |||||
| Pharmacist | X | X | |||||||
| Registered Dietitians | X | X | |||||||
| Counsellors | X | X | X | ||||||
| Psychiatrists | X | X | X | ||||||
| Psychologists/Mental Health Therapists | X | X | X | ||||||
| Podiatrists | X | X | |||||||
| Pedorthists | X | ||||||||
Note: The method of delivery of conservative OA treatments can vary between disciplines, between practices and between communities. Clinicians should talk with their individual with OA to make sure the referral will be the right fit for the individual.*Note: Clinicians can offer these services with the applicable training.