BEING ASSESSED FOR OA
STANDARD 1
For adults who present with the usual signs and symptoms of OA, a diagnosis can be made by having a complete clinical assessment.

OVERVIEW
- If you have joint pain (especially if you’re over 40), swelling or stiffness in your hips, knees, or lower back you should seek out a health care clinician for a complete examination – you may have OA
- Prepare for your visit by thinking about and writing down your medical history and writing down so you don’t forget anything when you see your clinician
- A complete clinical assessment for OA of the hip or knee is considered:
- reviewing your medical history
- ruling out other health conditions
- looking for other risk factors that may contribute to the development of the OA
- a physical exam to understand strength and presentation of the joint
- X-rays and lab tests usually don’t help to diagnose OA. What you see on x-ray doesn’t always match your symptoms
- Your experience with your symptoms in your joint (pain and ability to move) will guide your care plan
- You have a right to a respectful and culturally appropriate assessment and diagnosis
It’s important to be diagnosed early with osteoarthritis as the symptoms don’t go away and they don’t get better, especially if not treated. Developing ways or strategies to manage your osteoarthritis can slow the disease and the worsening symptoms.
- Reviewing your medical history
- Ruling out other health conditions
- Looking for other risk factors that may contribute to developing osteoarthritis
- A physical examination
SYMPTOMS
- Movement-related joint pain (not due to an injury) that doesn’t go away
- Aching
- Swelling
- A joint that ’catches’
- Joint stiffness in the morning that lasts less than 30 minutes
- A recent history of injury
- A joint that ‘locks’
- A joint that gives out
- Morning stiffness that doesn’t go away after 30 minutes
- Symptoms that came on quickly
- Joints that are hot and swollen
- You just don’t feel well
Your clinician will do more tests to find or to rule out other concerns, like an injured knee ligament, gout, inflammatory arthritis, or rheumatoid arthritis.
STAGES OF OA
You’ll hear terms like ‘early/mild’, ‘moderate’, or ‘advanced/late’ used to describe your osteoarthritis.
However, these 9 standards never use these terms to describe you and/or your treatment options. This is because the information in the standards can be adjusted to meet your needs for where you are right now. The toolbox of osteoarthritis treatments is for all stages of osteoarthritis.
These words are also unfair to describe where you are in your osteoarthritis journey. For example, if you’ve been managing your condition for some time your disease may be in the ‘early’ stage, but your journey may be ‘advanced’.
IMAGING
osteoarthritis: A systematic search and summary of the literature. BMC Musculoskeletal Disorders. 2008;9(1):1-11. doi: https://doi.org/10.1186/1471-2474-9-116. osteoarthritis. The clinical diagnosis is enough to begin planning your care and treating the osteoarthritis and your symptoms: Your pain or how well you can move the joint should guide how your osteoarthritis is managed. What’s seen on x-ray may not always match your symptoms. It also doesn’t predict how you’ll respond to your treatment.
Using x-rays to track how your osteoarthritis is progressing isn’t usually done. Your care plan should be guided by your symptoms and choices you’ve made through shared decision-making (SDM), Repeated x-rays don’t add anything to planning your treatment, unless your symptoms change suddenly or unexpectedly, and an x-ray hasn’t been done in 1 or 2 years.
ETHICS AND INCLUSIVITY
You have a right to a respectful and culturally appropriate assessment and diagnosis. You also have a right to a second opinion if you wish. Your clinical assessment should be complete to properly diagnose your condition.
Shared Decision Making
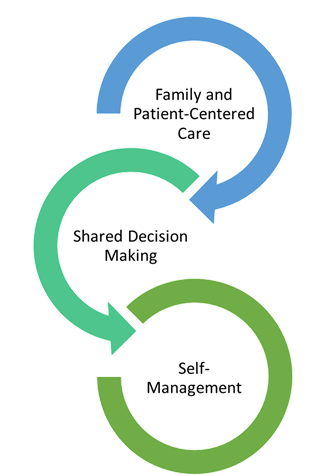
SDM
We mention evidence-based SDM techniques and processes a lot in these standards. SDM is an important part of family and patient-centred care. SDM is when you and your clinician share information and decide together what the best treatment option for you is. SDM is proven to lead to better outcomes for you, such as being satisfied with and having success with your care plan.
Standard 2 describes how sharing the decision-making is important for building a care plan.
OA Clinicians
- Family doctors
- Nurse practitioners
- Physiotherapists
- Occupational therapists
- Specialty physicians including:
- Sport and exercise medicine physicians
- Rheumatologists
- Physiatrists
- Chiropractors
- Orthopedic surgeons
Regulated Clinicians:
- Family physicians
- Nurse practitioners (NPs, RNs, LPNs)
- Physiotherapists (Allied Health)
- Occupational therapists (Allied Health)
- Pharmacists (Allied Health)
- Registered Dietitians (Allied Health)
- Psychiatrists
- Psychologists/Mental Health Therapists
- Specialty physicians including:
- Sport and exercise medicine doctors
- Radiologists
- Rheumatologists
- Physiatrists
- Chiropractors
- Orthopedic surgeons
Non-Regulated Clinicians:
- Podiatrists
- Pedorthists
- Kinesiologists
- Exercise physiologists
- Recreational therapists
- Counsellors