DEVELOPING A CARE PLAN
STANDARD 2
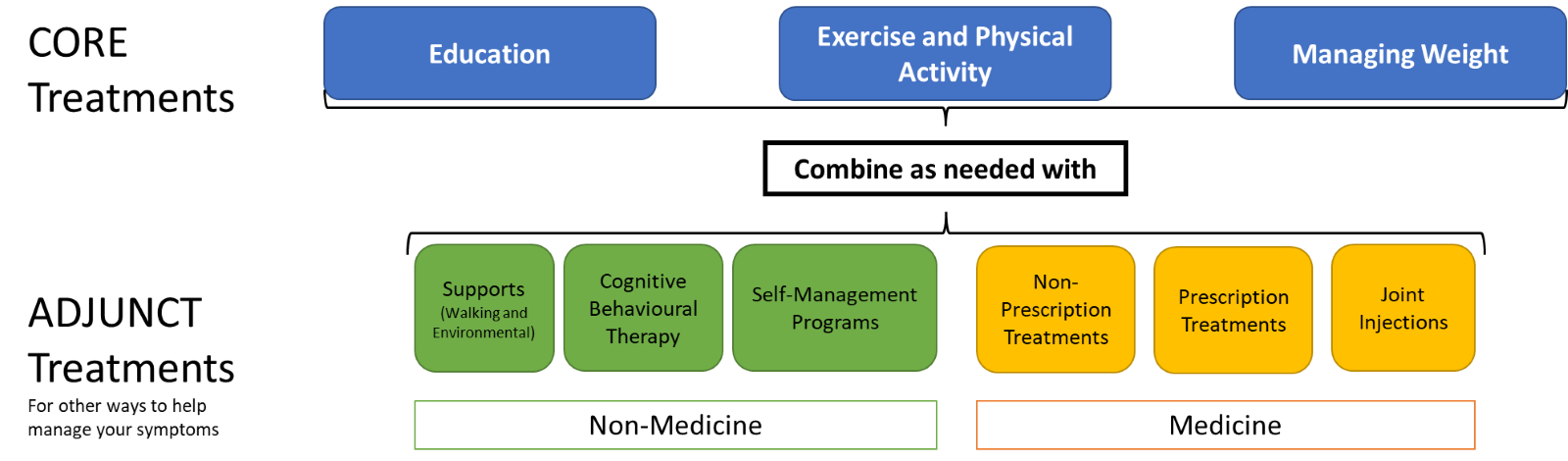
You and your clinician will develop a care plan by talking about the evidence based treatment options. Using the shared decision-making (SDM) approach will make sure your health priorities, goals, values, and preferences form the base of your care plan.

OVERVIEW
- A care plan is a living document that describes the treatments you and your primary clinician talk about and decide together to address your health concerns and goals
- Working with your clinician you can tailor your care plan to your needs and interests
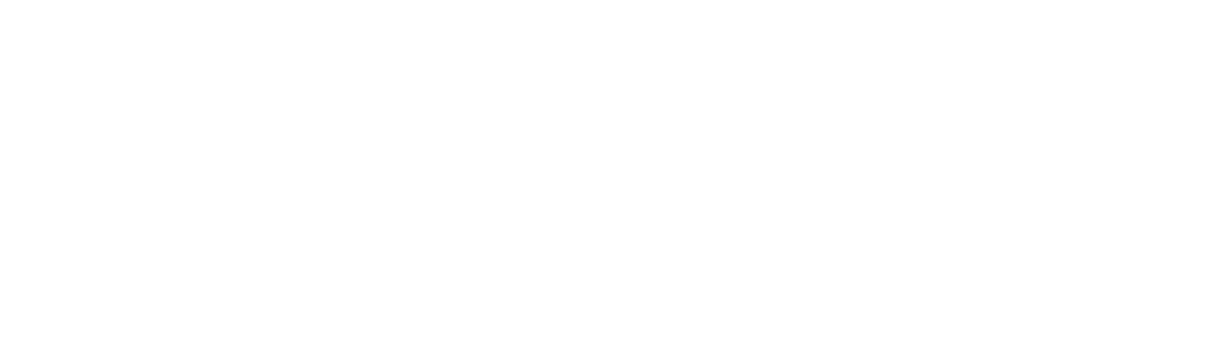
- Core Treatments have the strongest evidence for helping your OA. Adjunct Treatments support your Core Treatments.
- Choose 1-2 things to try at first, and work with your clinician to attach SMART goals to your choices
- Your OA Self-Management Toolkit gives you information and examples of treatments to try
- Ask for your Resource Inventory to learn where you can find treatments in your area
The osteoarthritis care plan describes the treatments you and your clinician talked about. They’re picked to focus on a range of items. A care plan will change as your condition and symptoms change. Standard 3 describes how to adjust or tailor your care plan over time after the first care plan is created. This is done to help manage your symptoms and prevent your osteoarthritis from progressing so that you have the best joint function possible.
You and your clinician will develop your care plan based on your:
Building an OA Care Plan
- Picking Core Treatment(s) that are tailored to your needs
- Picking a combination of Adjunct Treatment(s) to support the Core Treatments, if needed (Standard 7)
- Attaching SMART goal(s) to the selected treatment(s)
- Choosing a follow-up plan and revising the care plan as your needs and priorities change (Standard 3)
- Make sure the goals you set are meaningful to you
- Make you happier with your plan, which makes it more likely that you’ll follow it
- Increase the chance you’ll follow your care plan
2Gay C, Chabaud A, Guilley E, Coudeyre E. Educating patients about the benefits of physical activity and exercise
for their hip and knee osteoarthritis. Systematic literature review. Annals of Physical and Rehabilitation Medicine. 2016;59(3):174-83.
3Rice D, McNair P, Huysmans E, Letzen J, Finan P. Best evidence rehabilitation for chronic pain part 5: Osteoarthritis. Journal of Clinical Medicine. 2019;8(11):1769
4Wellsandt E, Golightly Y. Exercise in the management of knee and hip osteoarthritis. Current Opinion in Rheumatology. 2018;30(2):151-9.
As soon as possible after an osteoarthritis diagnosis, you’ll have:
- Education to give you the knowledge and skills that give you the confidence to learn about OA and the evidence-informed treatments available to you 11Bowden JL, Hunter DJ, Deveza LA, Duong V, Dziedzic KS, Allen KD, et al. Core and adjunctive interventions for osteoarthritis: Efficacy and models for implementation. Nature Reviews Rheumatology. 2020;16(8):434-47. (Standard 4)
- Exercise and physical activity to encourage you to use movement to improve your joint health and do your everyday activities 1,31Bowden JL, Hunter DJ, Deveza LA, Duong V, Dziedzic KS, Allen KD, et al. Core and adjunctive interventions for osteoarthritis: Efficacy and models for implementation. Nature Reviews Rheumatology. 2020;16(8):434-47.
3Rice D, McNair P, Huysmans E, Letzen J, Finan P. Best evidence rehabilitation for chronic pain part 5: Osteoarthritis. Journal of Clinical Medicine. 2019;8(11):1769(Standard 5) - Managing your weight to prevent increasing the load on your joint.1,31Bowden JL, Hunter DJ, Deveza LA, Duong V, Dziedzic KS, Allen KD, et al. Core and adjunctive interventions for osteoarthritis: Efficacy and models for implementation. Nature Reviews Rheumatology. 2020;16(8):434-47.
3Rice D, McNair P, Huysmans E, Letzen J, Finan P. Best evidence rehabilitation for chronic pain part 5: Osteoarthritis. Journal of Clinical Medicine. 2019;8(11):1769 This will affect your joint health and improve your ability to move so you can do your everyday activities (Standard 6)
Adjunct Treatments can also be tailored to your needs and preferences. They’re used to support you taking part in your Core Treatments (Standard 7). Some treatments will cost money, so speak with your clinician about what you’re able and willing to pay for.
The OA Self-Management Toolkit includes basic information about OA and 3 tools: 1. a Report Card, 2. a Treatment Menu and 3. an example of a Resource Inventory. These tools can support and encourage you to choose the treatment options you want and can help you manage your OA treatment plan over the long term.
Everyone with OA seeks care at different points in their OA journey. Talk to your clinician about how to try the treatments you choose together. Choosing 1 or 2 treatments to start with can prevent you from making too many changes at the same time. A good idea is to start with just 1 treatment within 3 months after your OA diagnosis.
Putting a Care Plan into Action
As soon as possible after an osteoarthritis diagnosis, you’ll have:
- Created and documented your care plan with your primary clinician
- Some ideas on things you can do (actions you can take) to begin your care plan
- Started at least 1 of the treatment options you’ve chosen
- A plan for following up with your clinician (Standard 3)
The exception to this is if you’re referred to an orthopaedic surgeon right away (your clinician will decide if this is right for you). If you do have to see a surgeon, an osteoarthritis treatment plan will include the surgeon’s recommendations. Standard 8 talks more about how surgery may only be one step in the ongoing journey in managing your osteoarthritis. It also talks about how surgery isn’t right for everyone.
Talk to your clinician about your follow-up plan. Standard 3 describes more about how to adjust your care plan on your osteoarthritis journey.

ETHICS AND INCLUSIVITY
You have a right to a respectful and culturally appropriate talk about your treatment options, and how it fits your cultural customs. You also have a right to tailor your care plan to your interests and what you’re able to do.
Managing Your OA
You understand that OA is a progressive disease with no cure. You live with your disease every day, while the clinicians provide support for short periods or short interactions. Throughout these 9 standards, the principles of self-management are reinforced. Confidence in self-management can be supported by the family and patient-centred care approach using SDM techniques.
All the processes and strategies described in these standards focus on supporting you as you learn more about your OA so you can have all the tools you need to make choices for your OA journey. The principles of self-management are vital to managing your symptoms day-to-day. Even when you’re doing everything ‘right’, OA can flare up for no reason that you can figure out. Once you understand this, and you have the tools you need, you’ll be ready to act when this happens.
SDM
As care progresses, every clinician should support your treatment and coping choices. Other ways to manage your coping strategies for OA include:
- setting your priorities and goals
- managing your symptoms
- hot and cold therapies
- selecting your own activities
- manging your mental health
- making clinician appointments as needed
There’s more information in Standard 7 if you want to become even more confident in your self-management techniques.
Your OA Self-Management Toolkit
The OA Self-Management Toolkit is designed for you. It’s evidence-based and can be adapted to many healthcare settings. You can use the toolkit to build a care plan and to update your care plan as your symptoms change.
The toolkit was designed with the principles of family and patient-centred care in mind. The tools are easy to use with SDM techniques to help you manage your OA. The toolkit was also created by people before you who also have OA.
| Education Booklet | Gives you the basic information about OA, from the basic facts to learning coping techniques. |
| Report Card | A one-time worksheet for you to write about the treatment options you’ve used so far and to identify your values and goals. |
| Treatment Menu | Lists examples of treatment options from the Core and Adjunct Treatments you can choose from. |
| Resource Inventory |
This tool tells you ‘where’ and ‘how’ you can trial your selected treatments. It’s an important part of putting your plan into action. Resource Inventories aren’t always available where you live so you want to make sure you keep this list up to date. A Resource Inventory specific to the area you live. This template helps you create a Resource Inventory specific to the area you live. |
Smart Goals
| S | Specific | The goal is specific to the OA treatment selected (e.g., going to the pool for aerobics). |
| M | Measurable | How often you’ll do the activity (e.g., going to the pool 2 days a week). |
| A | Attainable | The goal is chosen in context of your life (e.g., going to the pool 2 days a week is an important but realistic change from what you’re doing now and a there’s a pool near you). |
| R | Rewarding | The goal is meaningful to you. (e.g., going to the pool includes a chance to visit with a close friend and you’ll be working on changes for your OA together). |
| T | Timely | The goal has some due dates (e.g., pool visits start next week, and you and your primary clinician will review them in 4 weeks) |
SMART goals take practice to write. They’re the most successful when you and your clinician create them together.
Active vs Passive Treatment
SDM
When we talk about treatments, we usually mean the evidence-based options you have to manage your OA. However, treatments can also include a range of interactions between you and a clinician. For example, sometimes the clinician may suggest a pool therapy program and another time, you may be given an injection:
- Active treatments mean you’re a full participant in the treatment (e.g., pool therapy program).
- Passive treatments mean you receive something from a clinician (e.g., a joint injection).
Whether the treatments are active, passive, or a mix of the two, throughout these 9 standards the principles of family and patient-centred care are stressed to encourage using SDM techniques with you to support you to manage your OA.
Overall Well-Being
Overall Well-Being
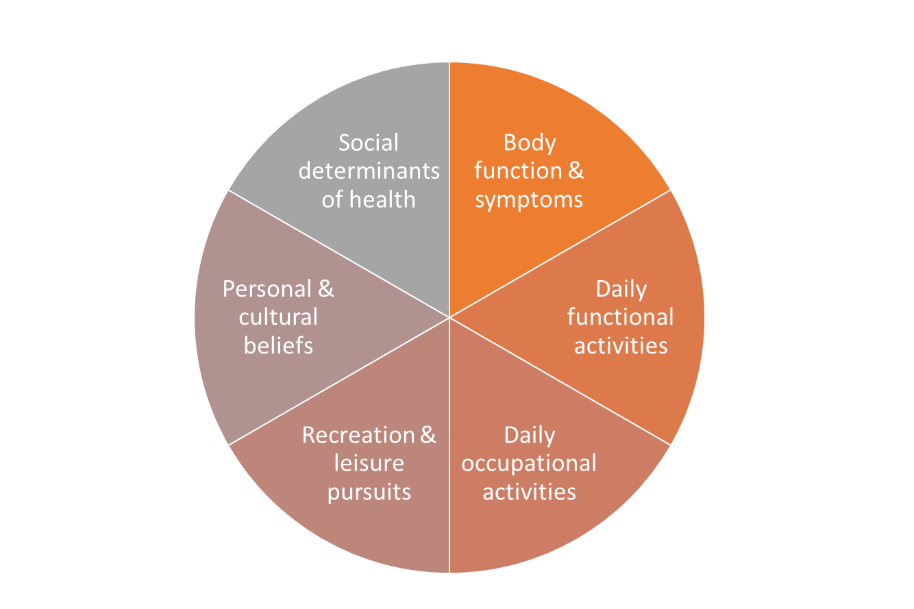
An OA management care plan considers your overall well-being. It includes many factors:
- Body function and symptoms such as pain, swelling, joint range of motion, strength, balance, and any other health issues you may have.
- Daily functional activities such as personal care, walking, climbing stairs, sleep, housework, and preparing meals.
- Daily occupational activities such as your job and family responsibilities.
- Recreation and leisure activities and interests.
- Personal and cultural beliefs and attitudes towards health, activity, and exercise.
- Social determinants of health including gender/gender identity, race/racialization, respectful and culturally appropriate care for Indigenous people, income/income security, employment/job security.
OA Self Management Toolkit
OA Self Management Toolkit, Includes: